Table Of Contents
-
Key Highlights:
-
Why Does Blood Sugar Control Matter During Pregnancy?
-
Normal Range Of Blood Sugar During Pregnancy: For Women Without Diabetes
-
Target Blood Sugar Levels In Expectant Mothers With Preexisting Diabetes
-
What Is Gestational Diabetes Mellitus & How Does It Affect Mothers-To-Be?
-
The Tests For Gestational Diabetes
-
How To Monitor Blood Glucose Levels During Pregnancy
-
Managing Healthy Blood Glucose In Pregnancy
-
Tips To Maintain Blood Sugar For Expectant Mothers
-
Postpartum Blood Sugar Care Guide For Both Mother & Baby
-
Frequently Asked Questions (FAQs)
-
Your Journey To A Healthy Pregnancy With MD Pilot
-
References:
Every meal, every craving, every test — pregnancy changes how your body handles sugar. But do you know what numbers are actually safe?
Knowing the normal range of blood sugar during pregnancy isn’t just trivia. It’s about safeguarding your baby’s healthy growth and protecting your own well-being. For instance, high or low levels can influence birth weight, delivery outcomes, and even your daily energy. With a clear sense of what’s normal, you gain confidence to make informed choices throughout your pregnancy journey.
This article will explain the normal blood sugar range during pregnancy, why it matters at each stage, and how you can monitor and manage it confidently. You will also learn actionable steps, research-backed tips, and an overview of the medical guidelines into clear steps for everyday use. So, let’s get into it.
Key Highlights:
- Knowing the normal range of blood sugar during pregnancy is crucial for protecting both maternal health and fetal development.
- High or low glucose levels can affect birth weight, delivery outcomes, and daily well-being.
- Gestational diabetes is common but manageable with clear targets, consistent testing, and lifestyle support.
- The recommended blood sugar targets vary for non-diabetic pregnancies, gestational diabetes, and preexisting diabetes, but all focus on maintaining safe ranges.
- Monitoring methods like fingerstick testing and continuous glucose monitoring (CGM) help expectant mothers stay on track.
- Balanced nutrition, controlled meal plan, safe exercise, stress management, and medication (when necessary) are key to stable blood sugar.
Why Does Blood Sugar Control Matter During Pregnancy?
During pregnancy, hormones like human placental lactogen, progesterone, and estrogen can make your body less sensitive to insulin. This means your blood sugar may run higher than usual, even if you didn’t have diabetes before. The effect is especially noticeable in the second and third trimesters. That’s why there are defined “normal” or “target” blood sugar ranges.

Research shows that moderate rises above these recommended levels can have measurable effects. For instance, every 1 mmol/L increase in the glucose after fasting is linked to a higher birth weight and a 1.35% rise in the risk of premature birth.
The good news is that most mothers-to-be manage hyperglycemia (high blood sugar) effectively with healthy eating, gentle exercise, and regular check-ups. In addition, balanced meals with protein help prevent spikes, while short walks after eating can lower post-meal glucose. This is generally enough to reduce high-risk factors and keep both mother and baby safe.
While high blood sugar carries certain risks, low blood sugar (hypoglycemia) brings its own challenges, especially for women taking insulin or other medications. Hypoglycemia can cause temporary symptoms like lightheadedness or fatigue, but these episodes are usually manageable with proper guidance. So, staying aware of the normal range of blood sugar during pregnancy helps prevent both extremes and supports optimal health.
Normal Range Of Blood Sugar During Pregnancy: For Women Without Diabetes
Guided by ACOG (American College of Obstetricians & Gynecologists) and other peer-reviewed studies, the target ranges are consistently associated with improved maternal and fetal outcomes. For pregnancies not related to diabetes, the normal range of blood sugar during pregnancy is as follows:
| Glucose Measurement | Blood Sugar Goal | When To Test |
|---|---|---|
| Fasting Blood Sugar or Pre-Meal | 70-95 mg/dL (3.9-5.3 mmol/L) | Upon waking up before eating |
| 1-Hour Post-Meal | <140 mg/dL (<7.8 mmol/L) | 1 hour after eating |
| 2-Hour Post-Meal | <120 mg/dL (<6.7 mmol/L) | 2 hours after eating |
| A1C Target | <6% (<42 mmol/mol) if it can be achieved without causing significant hypoglycemia, but it can be relaxed to <7% (<53 mmol/mol) when necessary to prevent low blood sugar | Every 2-3 months |
These guidelines provide a general framework, and individual targets may vary. Your doctor might recommend stricter or slightly relaxed ranges depending on factors such as prior diabetes history, the stage of pregnancy, overall health, weight, and family history. Remember that regular tracking can help guide lifestyle adjustments and provide helpful information for healthcare providers to maintain safe levels.
Target Blood Sugar Levels In Expectant Mothers With Preexisting Diabetes
The American Diabetes Association (ADA) has put together recommended blood glucose target ranges for pregnant women with type 1 or type 2 diabetes. Understanding the normal range of blood sugar during pregnancy helps mothers-to-be monitor their levels effectively, plan meals, and work closely with healthcare providers to maintain stable glucose throughout gestation.
| Glucose Measurement | Blood Sugar Goal For Type 1 Diabetes / Type 2 Diabetes |
|---|---|
| Fasting Blood Sugar or Pre-Meal | 70-95 mg/dL (3.9-5.3 mmol/L) |
| 1-Hour Post-Meal | 110-140 mg/dL (6.1-7.8 mmol/L) |
| 2-Hour Post-Meal | 100-120 mg/dL (5.6-6.7 mmol/L) |
| A1C Target | <6–6.5% (<42–48 mmol/mol) early in gestation, <6% (<42 mmol/mol) in the second and third trimesters |
What Is Gestational Diabetes Mellitus & How Does It Affect Mothers-To-Be?
Gestational diabetes mellitus (GDM) occurs when hormonal changes in pregnancy make the body less responsive to insulin. Consequently, glucose remains in the bloodstream rather than being used by cells for energy. Unlike type 1 diabetes, which results from insufficient insulin production, GDM is primarily caused by insulin resistance, with symptoms typically resolving after childbirth.
Every year, 5%-9% of pregnancies in the US are affected by GDM, and around 50% of these women are at risk of developing Type 2 diabetes later in life. While these numbers may sound concerning, with proper monitoring and care most women with GDM go on to have healthy pregnancies and babies when they follow proper medical guidance.
Although certain factors may slightly increase the risk. These include being overweight, family history of diabetes, previous delivery of a baby weighing over 9 pounds, and being over the age of 25. Following the normal range of blood sugar during pregnancy with gestational diabetes is a practical way to manage these risks effectively. The table below provides clear benchmarks for expectant mothers:
| Glucose Measurement | Blood Sugar Goal | |
|---|---|---|
| GDM (Gestational Diabetes Mellitus) Medicated With Insulin | GDM (Gestational Diabetes Mellitus) Not Medicated With Insulin | |
| Fasting Blood Sugar or Pre-Meal | 70-95 mg/dL (3.9-5.3 mmol/L) | <95 mg/dL (<5.3 mmol/L) |
| 1-Hour Post-Meal | 110-140 mg/dL (6.1-7.8 mmol/L) | <140 mg/dL (<7.8 mmol/L) |
| 2-Hour Post-Meal | 100-120 mg/dL (5.6-6.7 mmol/L) | <120 mg/dL (<6.7 mmol/L) |
The Tests For Gestational Diabetes
Early screening is essential to protect both mother and child. The ADA recommends testing women with diabetes risk factors during the first prenatal visit. For those without preexisting diabetes, GDM is typically identified between 24 and 28 weeks of pregnancy using specialized glucose tests. Postpartum screening is also recommended, with follow-up checks every three years to monitor for the development of type 2 diabetes.
According to the NIDDK guidelines, there are two tests for gestational diabetes: the Glucose Challenge Test (GCT) and the Oral Glucose Tolerance Test (OGTT). Women at higher risk may be tested earlier in pregnancy; in some cases, the OGTT may be performed without the GCT.
1. Glucose Challenge Test (GCT)
Often referred to as the glucose screening test, the GCT does not require fasting. The GCT process follows the steps below:
- A blood sample is drawn one hour after drinking the glucose solution offered by the healthcare professional
- If blood glucose is 140 mg/dL or higher, an OGTT is usually recommended
- A reading of 200 mg/dL or more may indicate type 2 diabetes, prompting further evaluation
2. Oral Glucose Tolerance Test (OGTT)
The OGTT provides a more detailed assessment. The steps involved in the process are as follows:
- Fast for at least eight hours before the test
- A baseline blood sample is drawn
- Drink a glucose-containing solution provided by the healthcare professional
- Blood samples are drawn at intervals (typically every hour for 2-3 hours)
- Elevated glucose levels at two or more times (fasting, 1-hour, 2-hour, or 3-hour) confirm a gestational diabetes diagnosis
How To Monitor Blood Glucose Levels During Pregnancy
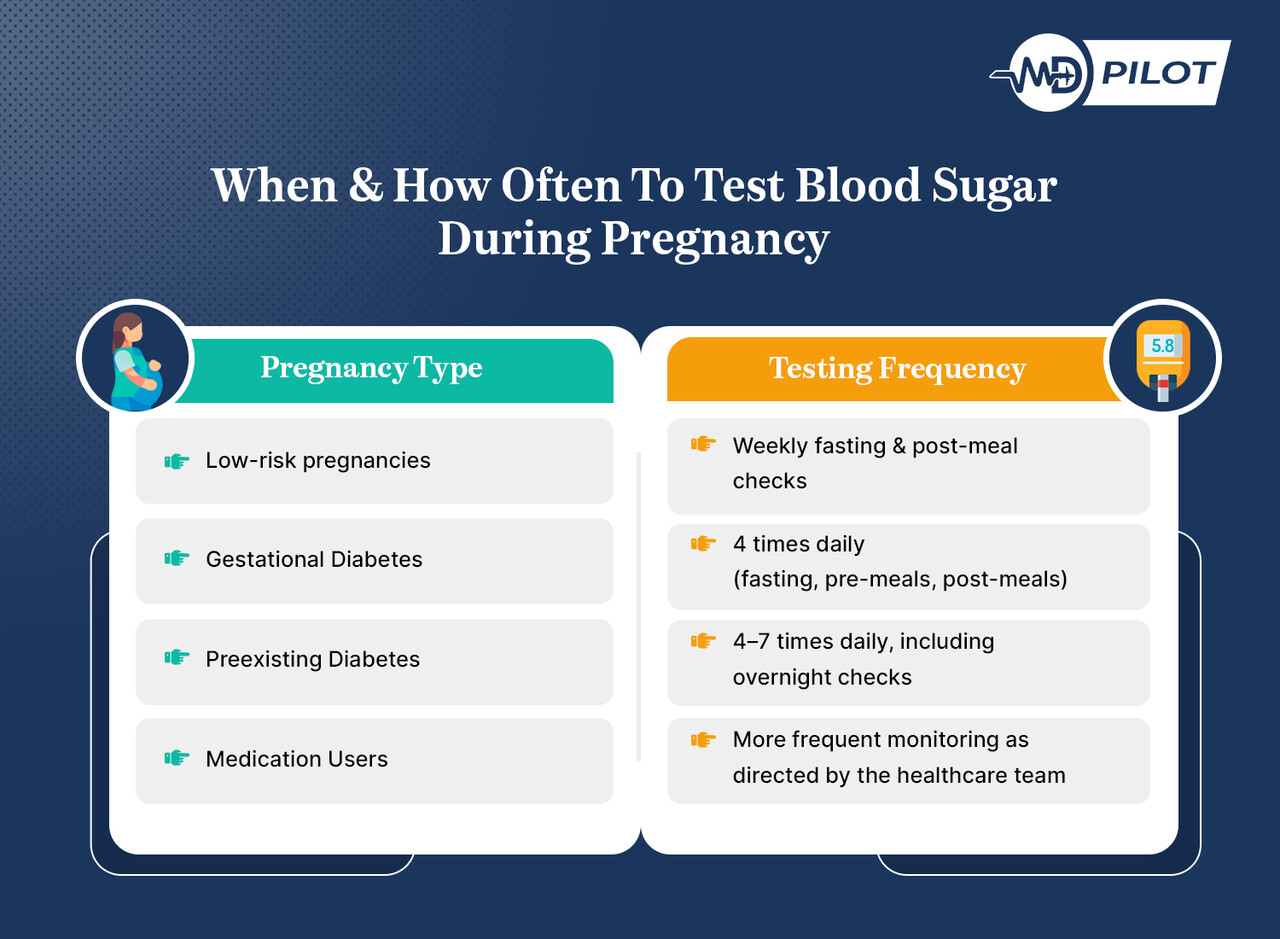
As pregnancy advances, insulin resistance naturally rises, necessitating more frequent testing. Maintaining readings within the normal range of blood sugar during pregnancy reduces complications and supports a healthier gestation. As a result, understanding traditional and modern monitoring approaches allows mothers-to-be to stay within target levels and make informed decisions about diet, activity, and treatment.
Traditional fingerstick testing remains widely used due to its affordability and accuracy. Typically, mothers check fasting blood sugar upon waking, before meals, 1–2 hours after eating, and at bedtime to monitor overnight trends. This method provides reliable measurements that help guide dietary adjustments and, if necessary, medication to maintain optimal glucose levels throughout pregnancy.
While fingerstick testing offers reliable snapshots, Continuous Glucose Monitoring (CGM) takes monitoring a step further by showing more detailed and real-time assessments throughout the day and night. CGM continuously tracks glucose trends, alerts users to dangerous highs or lows, and identifies patterns caused by meals or activity, allowing timely interventions for better management. The top three CGM metrics that are valuable during pregnancy are:
1. Time-In-Range (TIR)
This CGM metric shows the percentage of time glucose stays within the target range of 63–140 mg/dL. ADA recommends that pregnant women keep their Time-In-Range above 70%. More importantly, every 5% increase in TIR reduces the chances of newborn complications by 28%. This makes TIR a key metric for healthy pregnancy outcomes.
2. Time Above Range (TAR)
TAR, or Time Above Range, measures how long glucose has exceeded the safe level. Elevated TAR signals hyperglycemia (high blood sugar), which can increase complications during delivery. Identifying patterns that trigger TAR allows mothers and clinicians to adjust diet, activity, or medications and bring sugar levels back into the target range.
3. Time Below Range (TBR)
Time Below Range tracks periods of low glucose. Excessive TBR can result in hypoglycemia (low blood sugar), which can cause dizziness, fainting, or stress on the baby. CGM alerts on Time Below Range help prevent severe lows by prompting timely carbohydrate intake or medication adjustments.
| For Pregnant Individuals With Type 1 Diabetes | ||
|---|---|---|
| CGM Glucose Ranges | Metric | Blood Sugar Goal |
| 63–140 mg/dL (3.5–7.8 mmol/L) | Time-In-Range (TIR) | >70% |
| <63 mg/dL (<3.5 mmol/L) | Level 1 Time Below Range (TBR) | <4% |
| <54 mg/dL (<3.0 mmol/L) | Level 2 Time Below Range (TBR) | <1% |
| >140 mg/dL (>7.8 mmol/L) | Time Above Range (TAR) | <25% |
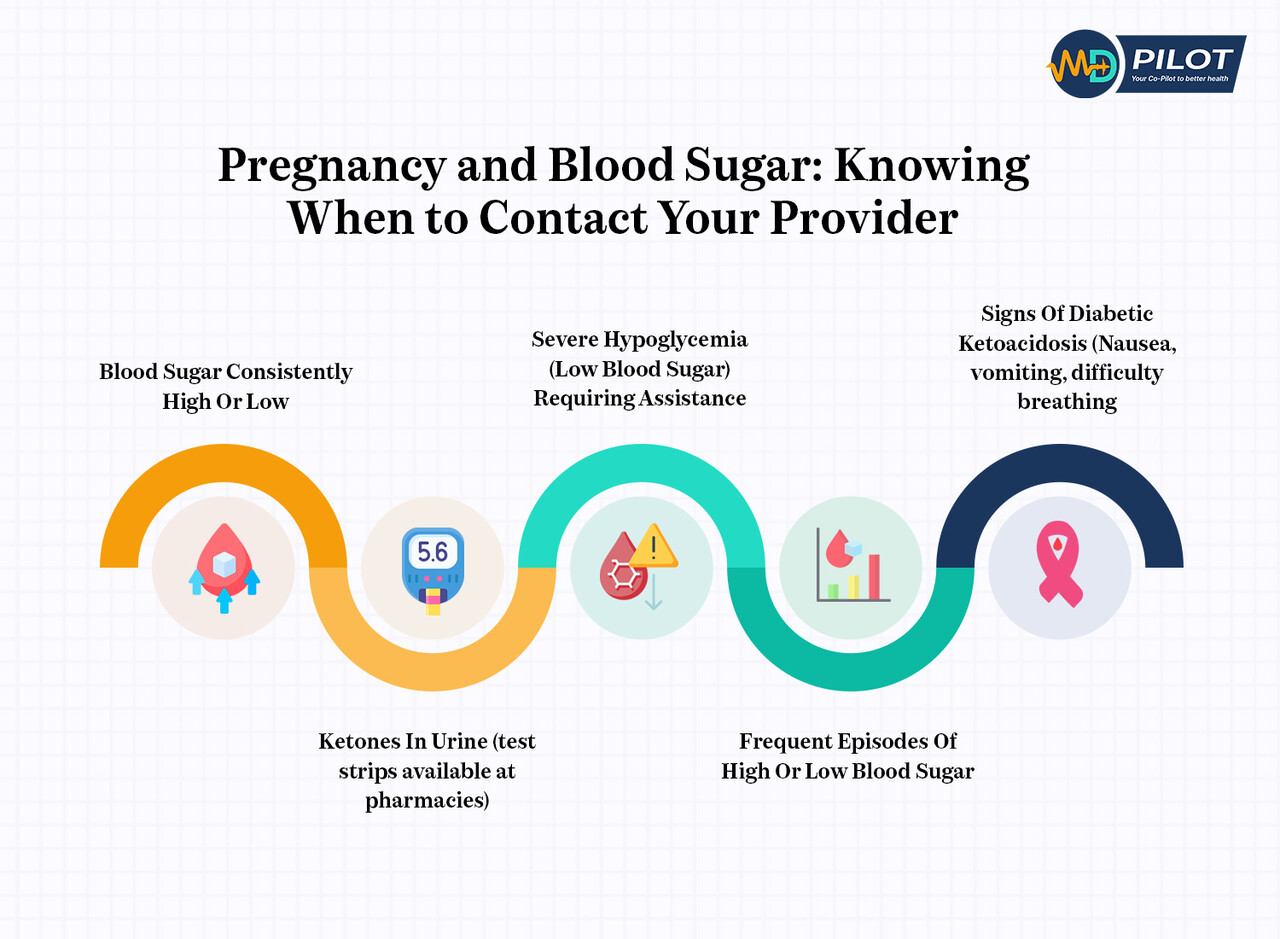
Managing Healthy Blood Glucose In Pregnancy
Monitoring and responding to fluctuations in blood glucose levels is vital for a healthy pregnancy. Occasional high or low readings do not automatically indicate a serious issue. Instead, consistent patterns over time matter most. Understanding these trends helps expectant mothers make informed decisions and maintain the normal range of blood sugar during pregnancy for optimal outcomes.
1. Gestational Diabetes Care
Managing GDM effectively relies on tailored lifestyle adjustments, including a balanced diet, portion control, and regular physical activity. For many pregnant individuals, these strategies alone may help achieve blood sugar targets. However, insulin therapy may be required if glucose remains outside the normal range. Remember that combining telehealth with in-person appointments can further enhance care outcomes.
2. Preexisting Diabetes Management
Insulin remains the primary treatment for type 1 or type 2 diabetes during pregnancy. Management options include multiple daily injections or insulin pump therapy for type 1 cases. In such cases, monitoring ketones and understanding diabetic ketoacidosis (DKA) prevention is necessary. Any additional medications must be carefully reviewed and prescribed only under close supervision by the healthcare professional overseeing the pregnancy.
3. Low-Risk Pregnancy Guidance
For women without GDM or preexisting diabetes, routine monitoring typically suffices. Blood sugar checks may occur during prenatal visits or through periodic home monitoring. In addition, maintaining a balanced diet, regular physical activity, and healthy weight gain supports keeping glucose levels within the normal range during pregnancy.
4. Medication & Glucose Monitoring
Pregnant women taking medications that may affect glucose require careful monitoring. Regular checks are crucial to ensure levels remain within the normal range of blood sugar during pregnancy. Keep in mind that healthcare providers may adjust dosages, substitute safer alternatives, or recommend additional testing to balance the benefits of treatment with maternal and fetal well-being.
Tips To Maintain Blood Sugar For Expectant Mothers
Successful blood sugar management during pregnancy revolves around four essential pillars: nutrition, physical activity, rest, and, when necessary, medication. Understanding these pillars allows you to create habits that steadily support healthy glucose levels. This approach also helps you consistently stay within the normal range of blood sugar during pregnancy, recommended by your healthcare provider.
1. Smart Food Choices
Focusing on consistent carbohydrate timing and quality rather than strict restriction works best for nutrition. Start by choosing complex carbohydrates (whole grains, legumes, and starchy vegetables) instead of simple sugars. Focus on fiber intake, aiming for 25–35 grams daily to regulate blood sugar naturally. Moreover, pair proteins with every meal and snack to slow glucose absorption.
2. Controlled Meal Plan
To build on smart food choices, maintain portion awareness using the plate method (half non-starchy vegetables, a quarter lean protein, and a quarter complex carbs). In addition, optimal meal timing matters. Eating smaller, more frequent meals and including snacks instead of long gaps can prevent glucose spikes, supporting a pregnancy-friendly blood sugar pattern.
3. Safe Exercise During Pregnancy
Physical activity is one of the most effective ways to support healthy glucose levels. For instance, walking 20–30 minutes after meals can significantly reduce post-meal glucose. Low-impact activities such as swimming, prenatal yoga, stationary cycling, and light strength training also improve insulin sensitivity, while being safe with proper modifications throughout pregnancy.
4. Low Stress & Enough Sleep
Next, don’t overlook stress management and sleep quality. High stress and poor sleep can raise glucose levels, undermining your efforts. Incorporating relaxation techniques, prenatal yoga, and regular sleep schedules helps improve insulin sensitivity. Combined with the dietary and exercise adjustments, these habits make staying within the normal range of blood sugar during pregnancy more achievable.
5. Medications, If Necessary
Sometimes, despite healthy eating and regular activity, blood sugar levels may still exceed targets during pregnancy. In such cases, your healthcare provider might consider medication, often starting with insulin. Any medication during pregnancy must be prescribed and supervised by a qualified healthcare professional to ensure the well-being of both mother and baby.
Postpartum Blood Sugar Care Guide For Both Mother & Baby
Blood sugar monitoring doesn’t end at delivery. Early postpartum screening, lifestyle support, and follow-up for both mother and baby are crucial. The points below combine widely accepted recommendations from leading authorities like ADA and ACOG into one easy checklist:
1. Early Postpartum Screening
Here are the key tests and follow-ups you can expect to discuss with your clinician in the first weeks after birth:
- A glucose test at 6–12 weeks postpartum using a 75-g oral glucose tolerance test (OGTT) or fasting plasma glucose (FPG) test as advised by your clinician
- If results are normal, continued screening every 1–3 years is required as part of lifelong surveillance
2. Management For Preexisting Diabetes After Birth
You can support a smoother recovery by keeping these management steps in mind:
- Expect insulin or other medication doses to decrease soon after delivery
- Increase self-monitoring of blood glucose, including nighttime checks if symptoms occur
- Schedule an early review (within days to weeks) to fine-tune targets and discuss contraception or future pregnancy plans
3. Lifestyle & Diabetes Prevention
These lifestyle moves can help lower your risk of future diabetes and speed up postpartum recovery:
- Enroll in structured weight-management or Diabetes Prevention Program–style interventions
- Follow a balanced eating plan designed by a dietitian
- Build at least 20-30 minutes of moderate physical activity into your everyday routine
4. Breastfeeding & Infant Follow-Up
Consider these practices to protect your health while supporting your baby’s growth and development:
- Breastfeeding is encouraged for its potential metabolic benefits to both mother and baby
- Inform your child’s healthcare provider about your diabetes history to track growth and metabolic risk
- Monitor your child’s growth and development for possible obesity or glucose intolerance
5. Education & Family Planning
Use these tips to stay informed, plan, and take control of your long-term health goals:
- Learn your personal risk for developing type 2 diabetes after GDM
Discuss contraception choices and timing of future pregnancies with your healthcare team
Keep a personalized record of test results, lifestyle goals, and upcoming appointments
Frequently Asked Questions (FAQs)
Managing glucose while expecting can feel overwhelming. Many individuals still have doubts after learning about targets, monitoring, and lifestyle tips. To make it easier, we have gathered the most common queries related to the normal blood sugar range during pregnancy, to help guide your everyday decisions.
Repeatedly over the target range readings, even if mild, may increase the risk of large birth weight, preeclampsia, or delivery complications. By reviewing your meals, adding moderate exercise, and following your health provider’s plan, you can often bring numbers back to target and effectively protect your health and your baby’s well-being.
To keep glucose steady, opt for balanced meals rich in complex carbohydrates, lean proteins, and healthy fats. Vegetables, nuts, seeds, and measured fruit portions help avoid spikes. Eating smaller portions more frequently, staying hydrated, and taking a gentle walk after meals naturally support healthier post-meal blood sugar patterns.
Yes, but with caution. HbA1C reflects average glucose over two to three months, yet pregnancy alters blood volume and red cell turnover, which reduces accuracy. It is most reliable as a supplement rather than a replacement for regular fasting and post-meal checks that give immediate insight into glucose trends.
Absolutely. Whole grains, legumes, and fiber-rich foods cause slower glucose rises than refined or sugary options. Considering both glycemic index and portion size helps smooth post-meal spikes. Pairing carbs with protein or healthy fats further stabilizes levels, supporting you in staying close to recommended glucose targets during pregnancy.
Your Journey To A Healthy Pregnancy With MD Pilot
Knowing the normal range of blood sugar during pregnancy is more than a medical guideline; it helps protect the mother’s health and support optimal fetal development. With clear targets, proactive monitoring, and the proper support, expecting mothers can reduce complications, feel more in control, and approach delivery with greater confidence and peace of mind.
At MD Pilot, we are dedicated to turning complex medical data into actionable and straightforward knowledge for mothers-to-be. Our pregnancy-focused portion calculator, glucose to HbA1c Estimator, and personalized diabetic snack builder help you and your care team stay aligned. They also make it easier to identify changes early and to base decisions on evidence rather than guesswork.
Using our tools and educational resources, you can actively monitor your glucose trends, understand what each reading means, and prevent spikes or dips before they become serious. These resources also strengthen your collaboration with healthcare professionals and safeguard your health and your baby’s development.
References:
- https://diabetesjournals.org/care/article/48/Supplement_1/S306/157565/15-Management-of-Diabetes-in-Pregnancy-Standards
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/gestational-diabetes
- https://www.cdc.gov/maternal-infant-health/pregnancy-diabetes/index.html
- https://med.uc.edu/depart/ob/divisions/mfm/diabetes-pregnancy-programs/about-high-and-low-blood-sugar
- https://www.niddk.nih.gov/health-information/diabetes/diabetes-pregnancy
- https://diabetes.org/living-with-diabetes/pregnancy/gestational-diabetes
- https://diabetesjournals.org/care/article/30/Supplement_2/S225/23894/Gestational-Diabetes-After-DeliveryShort-term
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5581263/
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




