Table Of Contents
-
Key Highlights
-
The Science Behind High Blood Sugar Levels And Headaches: Evidence & Complexity
-
Inside The Body: What Happens When Blood Sugar Stays High
-
Recognizing High Blood Sugar–Related Headaches: Symptoms & Patterns
-
Who Is At The Higher Risk Of High Blood Sugar Headaches?
-
How To Tell If Your Headache Is From High Or Low Blood Sugar
-
Headaches As A Warning Sign: Could It Be Diabetic Ketoacidosis (DKA)?
-
Strategies To Prevent & Manage Hyperglycemic Headaches
-
Managing High Blood Sugar Levels And Headaches In Kids
-
Frequently Asked Questions (FAQs)
-
MD Pilot Resources For Smarter Glucose & Headache Management
-
References:
It starts as a subtle pressure behind your eyes or a throbbing in your temples. The headache refuses to go away, no matter how much water or painkillers you take.
Could it be that this isn’t just stress, but your body signaling high blood sugar (a condition known as hyperglycemia)? Even if it seems minor, ignoring these headaches can be risky. They often indicate that your body is struggling to manage hyperglycemia, a warning you shouldn’t overlook.
Typically, they indicate underlying metabolic stress, vascular changes, or dehydration resulting from elevated glucose levels. Recognizing these early signs is the first step toward understanding what’s happening inside your body and taking proactive measures.
This guide will explore the relation between high blood sugar levels and headaches, highlight the signs to watch for, and share tips to reduce their frequency and severity. By the end, you will gain insights to understand, manage, and prevent these warning signals effectively.
Key Highlights
- Headaches that don’t respond to rest or hydration may be an early sign of high blood sugar, indicating that your body is under metabolic stress.
- Research links high glucose levels to vascular changes, dehydration, and disrupted brain energy use, all of which can trigger headaches.
- Recognizing patterns between meals, stress, and glucose readings helps you prevent recurring headaches.
- Managing hydration, eating balanced meals, regularly monitoring glucose levels, and controlling stress can help reduce both headache frequency and blood sugar spikes.
- Ignoring persistent sugar-related headaches can increase the risk of complications like diabetic ketoacidosis (DKA), especially if symptoms include thirst, fatigue, or blurred vision.
The Science Behind High Blood Sugar Levels And Headaches: Evidence & Complexity
The link between high blood sugar levels and headaches remains a topic of ongoing research, with varying studies yielding mixed results. A few notable studies on the connection between the two, highlighting the complexity, are as follows:
1. A Higher Headache Risk In People With Diabetes
A population-based study suggests that people with diabetes are more likely to experience headaches or migraines. This association is thought to arise because prolonged high blood glucose levels can affect blood vessels and cause nerve damage, thereby creating conditions conducive to headaches.
2. Contrasting Findings In Long-Term Studies
However, the picture becomes more complex when looking at long-term research. One study involving women found that those who suffered from regular migraines were actually less likely to develop type 2 diabetes later in life. This finding suggests that the relationship between migraines and blood sugar is not entirely linear and may involve other protective or compensatory mechanisms in the body.
3. Possible Shared Metabolic Factors
Adding another layer of complexity, another research has observed that individuals with migraines often have higher blood sugar levels during fasting compared to those without headaches. These findings hint at the possibility of a shared metabolic factor, such as insulin resistance, that could simultaneously influence both blood glucose regulation and migraine susceptibility.
4. Clinical Observations Highlighting Blood Sugar Control
Interestingly, a couple of medical case reports provide yet another perspective. They note that diabetic patients who achieved better blood glucose control—particularly through insulin therapy—experienced a noticeable reduction in migraine frequency. This observation underscores the potential role of glucose regulation in mitigating headache activity, even if a direct causal link remains unproven.
So, while the overall evidence doesn’t draw a direct line, it strongly suggests that glucose levels can influence headache activity. Even without definitive proof, these findings suggest that higher blood sugar levels can affect how the brain and blood vessels function. In the following section, we explore how elevated glucose levels may trigger these effects through multiple biological processes.
Inside The Body: What Happens When Blood Sugar Stays High
When blood sugar levels remain high for extended periods, the body responds in several ways that can contribute to headache pain. These changes often overlap and build on one another, affecting hydration, blood flow, hormones, and even how the brain uses energy. Here’s how those mechanisms unfold:
1. Dehydration & Fluid Loss
When glucose levels are too high, the body attempts to eliminate the excess sugar through urination. This leads to more trips to the bathroom and a loss of fluids, which can cause dehydration. One study even mentions that dehydration is among the most common triggers for headaches, linking fluid loss directly to headache severity.
2. Vascular & Hormonal Changes
High blood glucose can cause blood vessels to constrict or dilate unpredictably. At the same time, it can trigger the release of stress hormones, such as cortisol and adrenaline, which affect blood flow to the brain. Research has shown that blood sugar levels tend to rise during migraine attacks compared to normal periods, highlighting the interplay between vascular changes and headache onset.
3. How The Brain Uses Energy
The brain depends on glucose for energy. But when sugar levels rise and fall rapidly, or when insulin isn’t working as it should, brain cells don’t get a steady supply. One study points out that such fluctuations can make nerve cells more sensitive, which may trigger headaches or exacerbate existing ones.
4. The Stress Cycle
Headaches themselves can increase stress, which causes the body to release more cortisol and inflammation-related chemicals. Some research suggests that these stress responses can elevate blood sugar further, creating a cycle where stress and glucose feed into each other.
5. The Sugar Crash
Sometimes after a big sugar spike, the body releases more insulin than needed, causing blood sugar to drop suddenly — a “sugar crash.” This dip can also bring on a headache. Studies note that many people notice headaches both after skipping meals and after consuming large amounts of sugar at once, linking rapid blood sugar changes to headache onset.
Recognizing High Blood Sugar–Related Headaches: Symptoms & Patterns
Headaches associated with hyperglycemia often present with accompanying signs of elevated glucose levels. Some typical signs include:
| Symptom | Why It Matters | What To Observe |
|---|---|---|
| Headache accompanying thirst, frequent urination, fatigue | Suggests hyperglycemia | Check your blood sugar around the headache episode |
| Post-meal headache (1–2 hr after high-carb meal) | May relate to sugar crash or surge after eating | Note dietary patterns and timing |
| Persistent dull, bilateral ache affecting both sides of the head (temples or forehead) | Common form of “sugar headache” | Often relieved when glucose normalizes |
| Throbbing or dull headache | Caused by changes in blood vessel tone and dehydration from high glucose | May worsen with exertion or improve after hydration and glucose correction |
| Headache with blurred vision | Can indicate severe hyperglycemia or fluctuating blood sugar affecting eye fluid balance | Check your blood sugar immediately and seek medical attention if vision changes persist |
| Headaches that worsen as glucose remains uncontrolled | May indicate the body is under strain from continuous high blood sugar | Monitor glucose trends over hours/days |
| Headache without hyperglycemic symptoms | Suggests alternative cause | Check for high blood pressure, vision, neurological signs |
Who Is At The Higher Risk Of High Blood Sugar Headaches?
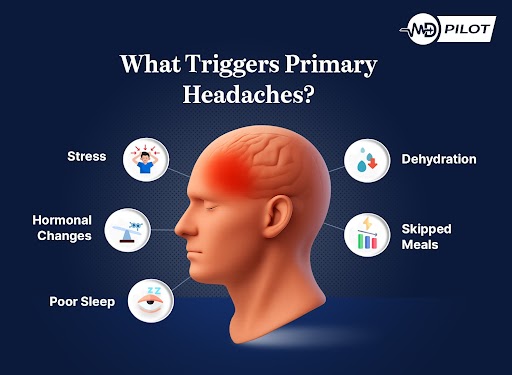
Understanding the factors that increase your susceptibility can help you prevent or reduce the discomfort associated with high blood sugar levels and headaches. By identifying these triggers, you can take proactive steps to manage your blood sugar and protect your well-being. Risk factors that increase the likelihood of hyperglycemic headaches are as follows:
- Existing diabetes, prediabetes, or impaired glucose tolerance
- Skipping or inconsistent use of diabetes medications
- High-glycemic diet (refined sugars and processed carbs)
- Poor hydration or excessive urination
- Irregular eating habits (skipping meals, swings in glucose)
- Stress, illness, and the use of certain anti-inflammatory medications such as corticosteroids
- Insulin resistance, obesity, or metabolic syndrome
How To Tell If Your Headache Is From High Or Low Blood Sugar
Understanding whether high or low blood sugar levels cause your headache helps you take the proper corrective action. Here’s how they differ:
| Aspect | Low Blood Sugar (Hypoglycemia) | High Blood Sugar (Hyperglycemia) | Why It Matters |
|---|---|---|---|
| Typical Cause | Blood glucose drops too low (below 70 mg/dL) due to missed meals, excess insulin, or heavy exercise | Glucose levels rises too high (above 180 mg/dL) from overeating, stress, illness, or inadequate medication | Correct identification helps avoid worsening either condition |
| Type of Headache | Dull, pressure-like, or pounding headache that may come on suddenly | Throbbing or persistent dull ache that builds up gradually | Treatment differs — sugar intake helps low blood sugar, but worsens in case of high blood glucose levels |
| Associated Symptoms | Shakiness, sweating, hunger, dizziness, irritability, blurred vision | Extreme thirst, frequent urination, fatigue, dry mouth, blurred vision | Recognizing other clues helps pinpoint the true cause |
| Timing | Usually appears when meals are delayed or after intense activity | Often follows heavy meals or prolonged stress | Noting the timings can guide prevention strategies |
| Relief Measures | Consume 15 grams of sugar (glucose tablets or fruit juice) and recheck levels in 15 min | Hydrate well, avoid sugary foods, take prescribed medications, seek medical attention if needed | Taking the wrong step can make symptoms worse |
| Risks If Ignored | Severe hypoglycemia can cause confusion, fainting, or seizures | Persistent hyperglycemia can cause kidney, eye, and nerve damage | Early correction prevents complications |
Headaches As A Warning Sign: Could It Be Diabetic Ketoacidosis (DKA)?
While headaches from high blood glucose are often linked to dehydration or vascular changes, they can sometimes signal a more serious complication: diabetic ketoacidosis (DKA). According to the American Diabetes Association (ADA), DKA occurs when the body lacks sufficient insulin to utilize glucose for energy.
In response, it begins breaking down fat, producing ketones as an alternative fuel. High ketone levels make the blood acidic, which can poison the body if left untreated. Although DKA is a serious condition, it is also highly manageable when detected and treated early. Regular blood sugar and ketone monitoring, along with prompt medical care, dramatically reduces risks and improves outcomes.
Early symptoms of DKA include:
- Excessive dry mouth or thirst
- Elevated blood glucose levels
- Frequent urination
- High ketone levels in the urine
As DKA progresses, other symptoms can develop, which are as follows:
- Persistent fatigue or weakness
- Flushed or dry skin
- Nausea, abdominal pain, or vomiting (contact a healthcare provider if vomiting lasts more than two hours)
- Fruity-smelling breath
- Difficulty breathing
- Confusion or having a hard time concentrating
Treatment typically occurs in a hospital, where fluids, insulin therapy, and electrolyte management help restore balance safely and effectively. While DKA can be life-threatening, understanding the warning signs and seeking timely care can prevent severe complications. Even something as simple as monitoring high blood sugar levels and headaches may serve as an early alert, giving you the chance to act before the situation escalates.
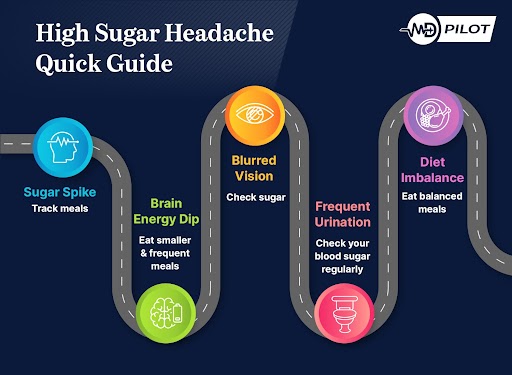
Strategies To Prevent & Manage Hyperglycemic Headaches
If you notice a pattern linking your headaches to high blood sugar, here are steps you can take to reduce both severity and frequency:
1. Stabilize Glucose Fluctuations
Here are a few dietary steps you can follow to stabilize your glucose levels:
- Eat consistent, balanced meals; avoid large glycemic “spikes”
- Prefer low-glycemic-index carbohydrates and pair with protein and healthy fat
- Avoid extended fasting or irregular meal timing
- If you are on glucose-lowering therapy, check whether your insulin or medication dosing contributes to rebounds
- Mind caffeine intake, which can affect blood sugar and worsen headaches
- Include magnesium-rich foods like spinach, almonds, and beans, as it may help reduce headache frequency
2. Hydrate Proactively
Since hyperglycemia promotes fluid loss, it is essential to stay well-hydrated. Drink ample water and electrolyte-balanced fluids at regular intervals. Moreover, limit sugary beverages as they can worsen hyperglycemia and dehydration.
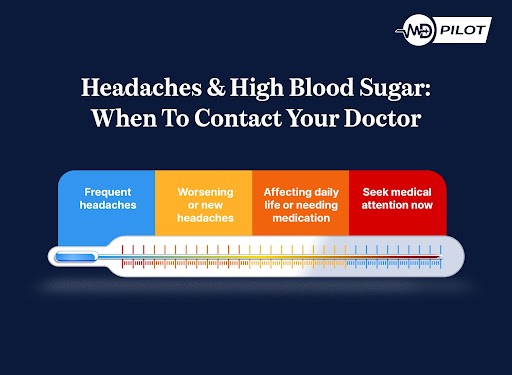
3. Frequent Monitoring
You can utilize a glucometer or continuous glucose monitor (CGM) to detect patterns (such as spikes or dips) that correlate with headache onset. This helps you intervene early. Keep in mind that environmental triggers, such as extreme heat, bright light, or prolonged screen time, may exacerbate headaches in conjunction with fluctuations in glucose levels.
4. Lifestyle Interventions
Here are a few lifestyle improvements that you can make to manage hyperglycemia:
- Incorporate regular physical activity to improve insulin sensitivity
- Poor sleep heightens metabolic stress and headache vulnerability, so ensure quality rest
- Manage stress to moderate hormonal triggers using breathing exercises, yoga, and cognitive techniques
- Optimize posture and workstation environments, especially if you spend long hours at a desk, as poor posture can intensify headache pain
- Limit alcohol and avoid tobacco, both of which can exacerbate headaches and affect glucose control
5. Track & Adjust With Data
Maintain a headache log that is aligned with glucose readings, sleep patterns, and stress levels. Include the timing of medications, meals, and physical activity, as these can reveal subtle patterns that trigger headaches. Then, look for clusters or patterns you can modify or bring up to your healthcare provider for a treatment plan.
Managing High Blood Sugar Levels And Headaches In Kids
Children may experience high blood sugar differently from adults, and recognizing early warning signs is crucial for their safety and well-being. Parents and caregivers should watch for the following indicators and take appropriate action:
- Frequent Urination & Excessive Thirst: A child who frequently asks for water or needs to use the bathroom often may indicate high blood sugar.
- Headaches or Complaints Of Head Pressure: Younger children may have difficulty describing pain, so irritability, fussiness, or withdrawal can be clues.
- Blurred Vision: Fluctuating blood sugar levels can disrupt the fluid balance in the eyes, leading to temporary vision issues.
- Fatigue or Reduced Concentration: May appear as tiredness or difficulty focusing in school.
- Nausea, Vomiting, or Abdominal Pain: Any of these can accompany hyperglycemia or indicate early diabetic complications.
- Unexplained Weight Loss: Persistent high blood sugar may cause rapid weight changes.
To manage your blood sugar and prevent any risks, you can consider the following tips:
- Monitor Glucose Levels Carefully: Use pediatric-appropriate devices and track levels consistently.
- Hydration & Balanced Meals: Encourage regular meals balanced with carbohydrates, proteins, and healthy fats.
- Regular Activity & Sleep: Support overall blood sugar stability.
- Maintain A Symptom Diary: Track headaches, meals, glucose readings, and behavior changes to identify patterns.
If any symptoms persist, worsen, or your child shows unusual changes in behavior or health, consult a pediatrician promptly for professional guidance.
Frequently Asked Questions (FAQs)
Understanding the nuances of headaches related to glucose fluctuations can be challenging. To clarify common concerns and provide practical guidance, we have compiled answers to frequently asked questions about high blood sugar levels and headaches:
The speed of relief can vary from person to person. Some individuals notice improvement within 30–60 minutes after their glucose levels stabilize. However, others may take longer, especially if dehydration, inflammation, or prolonged hyperglycemia contributed. Monitoring symptoms alongside glucose readings can help identify patterns and provide insight into underlying causes.
Occasional and mild use of painkillers may be acceptable. However, relying on painkillers frequently without addressing the root cause is not recommended. Persistent or recurring headaches should prompt a more thorough evaluation, ideally alongside glucose monitoring, to determine whether underlying metabolic factors or other health issues are contributing.
Migraines typically involve pulsatile pain, often on one side of the head, combined with sensitivity to light or sound, nausea, or aura. In contrast, sugar-related headaches tend to be dull, bilateral, and closely linked to fluctuations in glucose levels. Recognizing these differences can help tailor treatment and lifestyle adjustments effectively.
Yes, elevated glucose can trigger headaches in anyone, not just people with diabetes. Large intakes of sugar or refined carbohydrates, illness, or prediabetes can all contribute. Frequent headaches accompanied by thirst or increased urination may indicate a metabolic imbalance. Awareness of high blood sugar levels and headaches is essential for early intervention and prevention.
MD Pilot Resources For Smarter Glucose & Headache Management
The direct connection between high blood sugar and headaches might be ongoing but they are often an early signal that your body’s glucose balance is disrupted. Recognizing these warning signs and understanding the physiological connections allows you to take meaningful steps to reduce headache frequency and support overall metabolic health.
However, being aware of these patterns is only the first step. To make informed decisions and act effectively, having reliable data and guidance is crucial. Tools that track glucose trends and interpret fluctuations can bridge the gap between awareness and actionable steps, helping you understand how daily habits impact your well-being.
To translate insights into measurable progress, MD Pilot offers crucial health management resources. Our tools, such as the Blood Sugar Level Interpreter and the 7-Day Blood Sugar Tracker, provide insight into your glucose trends, highlight patterns, and help you take preventive measures. With these tools, you gain confidence, clarity, and proactive control over your metabolic health.
References:
- Del Moro, L., Rota, E., Pirovano, E., et al. (2022). Migraine, Brain Glucose Metabolism and the “Neuroenergetic” Hypothesis: A Scoping Review. The Journal of Pain, 23(8), 1294–1317.
https://www.sciencedirect.com/science/article/pii/S1526590022000396 - Florida Endocrinology And Diabetes Center. (2025). Diabetes and headaches: What’s the connection?
https://tampabayendocrine.com/diabetes-and-headaches/ - American Diabetes Association. (n.d.). Diabetes & DKA (Ketoacidosis).
https://diabetes.org/about-diabetes/complications/ketoacidosis-dka/dka-ketoacidosis-ketones - Hufnagl, K. N., & Peroutka, S. J. (2002). Glucose regulation in headache: implications for dietary management. Expert Review of Neurotherapeutics, 2(3), 311–317.
https://pubmed.ncbi.nlm.nih.gov/19810862/ - Children’s Healthcare of Atlanta. (n.d.). How Do You Spot Hyperglycemia in Children with Diabetes?
https://www.choa.org/parent-resources/diabetes/hyperglycemia-in-children - Islam, M. R., & Nyholt, D. R. (2022). Glucose-Related Traits and Risk of Migraine—A Potential Mechanism and Treatment Consideration. Genes, 13(5), 730.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9141901/ - U.S. National Library of Medicine. (n.d.). Blood Glucose. MedlinePlus.
https://medlineplus.gov/bloodglucose.html - Centers for Disease Control and Prevention. (2024). Your Brain and Diabetes.
https://www.cdc.gov/diabetes/diabetes-complications/effects-of-diabetes-brain.html - Zhang, D. G., Amin, F. M., Guo, S., et al. (2020). Plasma Glucose Levels Increase During Spontaneous Attacks of Migraine With and Without Aura. Headache: The Journal of Head and Face Pain, 60(4), 655–664.
https://pubmed.ncbi.nlm.nih.gov/32031249/
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




