Table Of Contents
-
Key Highlights
- Inside Your Numbers: What Glucose & A1C Really Reveal
- Common Blood Sugar Tests & When They’re Used
-
Risks of High & Low Blood Sugar
-
How to Keep Blood Sugar Levels in a Healthy Range (Management Plan)
-
Frequently Asked Questions (FAQs)
-
Mastering Your Blood Sugar Starts Here
-
List of References:
Your blood sugar levels tell a powerful story about your health.
Every day, your body regulates the amount of glucose in your blood to fuel energy, support brain function, and keep organs working properly. But when those numbers drift outside the target range, the risks grow. Persistent high blood sugar can lead to type 2 diabetes and long-term complications, while repeated lows can disrupt daily life and cause dangerous episodes.
That’s why understanding a chart of normal blood sugar levels matters. Whether you’re living with diabetes, at risk, or simply curious about your health, knowing how different tests measure your numbers helps you see the bigger picture and make informed choices.
Key Highlights
- A chart of normal blood sugar levels shows diagnostic cutoffs for diabetes and management targets for people already diagnosed.
- Diagnostic criteria: FPG <100 mg/dL is normal, 100–125 mg/dL is prediabetes, and 126 mg/dL or higher indicates diabetes.
- Management targets (for people with diabetes): 80–130 mg/dL before meals, <180 mg/dL two hours after meals, and A1C typically <7%.
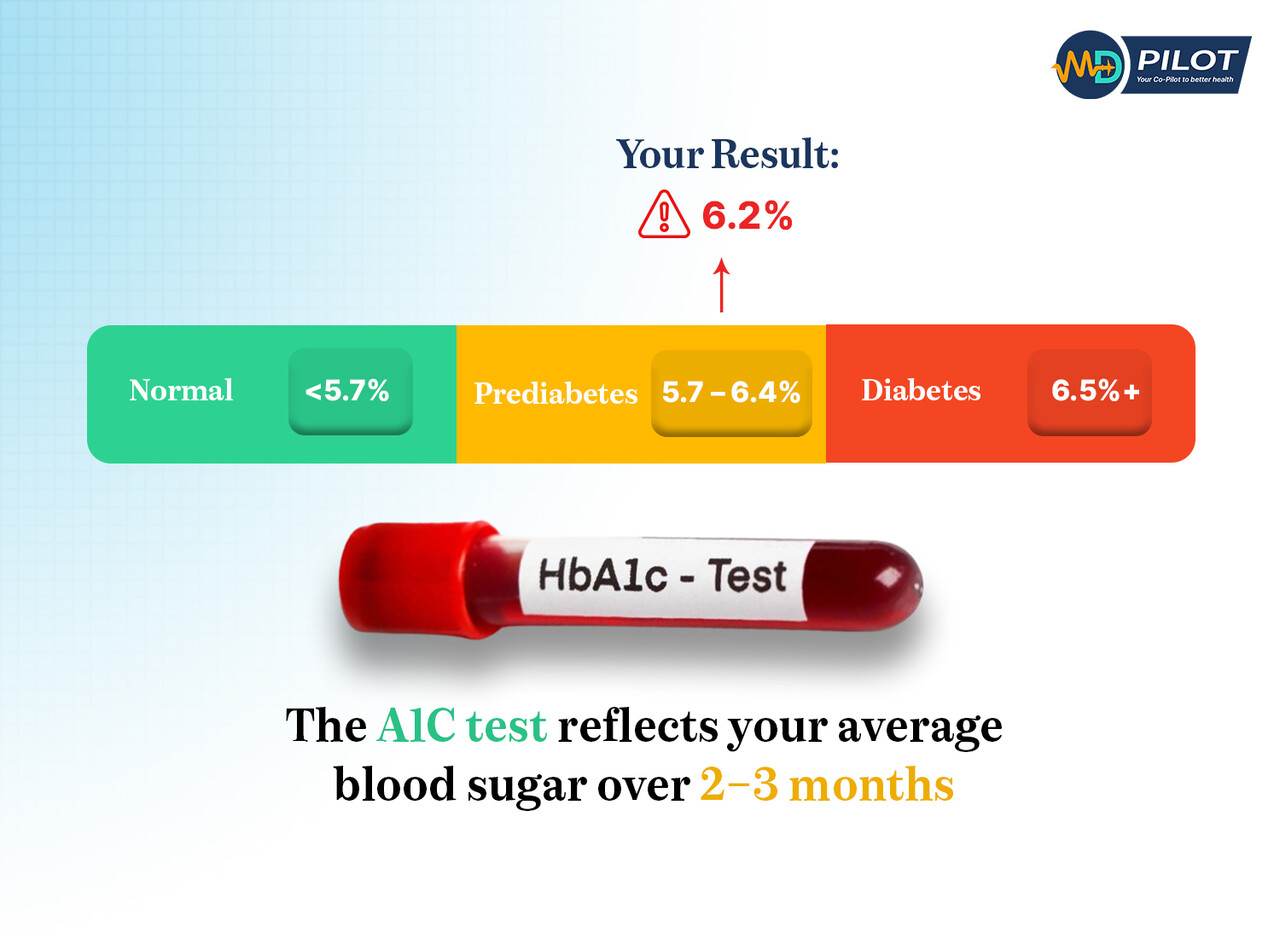
- The A1C test reflects your average blood sugar over 2–3 months and helps healthcare professionals track long-term stability.
- Levels outside the target range may lead to serious complications, but lifestyle changes, glucose monitoring, and a tailored management plan reduce risks.
- Work with healthcare professionals to individualize goals, since targets vary by health conditions, age, and treatment needs.
Inside Your Numbers: What Glucose & A1C Really Reveal
The Role of Glucose in the Body
Glucose is your body’s main fuel source. After eating, carbohydrates break down into glucose, which enters your bloodstream. Insulin, produced by the pancreas, moves this glucose into your cells for energy. When insulin doesn’t work properly — a common issue in people with diabetes — glucose builds up in the blood instead of being used effectively.
Over time, consistently high readings increase the risk of complications, including nerve damage, kidney disease, and heart problems.
The Importance of the A1C Test
Single blood sugar tests only measure your level at one moment in time. The A1C test, however, reflects your average blood sugar over the past two to three months by measuring how much glucose has attached to your red blood cells.
- Normal: Below 5.7%
- Prediabetes: 5.7%–6.4%
- Diabetes: 6.5% or higher
For adults with diabetes, many healthcare professionals recommend aiming for an A1C under 7% as part of a personalized management plan. Still, goals may differ based on age, other health conditions, or guidance from your care team.
Common Blood Sugar Tests & When They’re Used
Checking your blood glucose levels can mean different things depending on the test. Some measure your number at a single moment in time, while others show long-term patterns. The American Diabetes Association (ADA) 2025 Standards of Care and the Centers for Disease Control and Prevention (CDC) recognize four main tests:
1. Fasting Plasma Glucose (FPG) Test
- When it’s used: After at least 8 hours without eating or drinking anything other than water.
- Diagnostic ranges:
- Normal: 70–99 mg/dL
- Prediabetes: 100–125 mg/dL
- Diabetes: 126 mg/dL or higher
- Why it matters: The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) highlights this as one of the simplest, most common ways to detect early changes in blood sugar.
2. Oral Glucose Tolerance Test (OGTT)
- When it’s used: Often during pregnancy to detect gestational diabetes, or in situations where more detail is needed about how your body handles a set amount of glucose. After fasting, you drink a sweet liquid and your blood is tested 2 hours later.
- Diagnostic ranges (2 hours post-drink):
- Normal: Below 140 mg/dL
- Prediabetes: 140–199 mg/dL
- Diabetes: 200 mg/dL or higher
- Note: For adults with diabetes, the management goal is typically to keep levels below 180 mg/dL two hours after meals, but your provider may recommend a different target range based on age or other health conditions.
3. Random Plasma Glucose Test
- When it’s used: Taken at any time of day, regardless of when you last ate. Often used if symptoms suggest diabetes.
- Diagnostic threshold: 200 mg/dL or higher, combined with symptoms like excessive thirst, urination, or fatigue, indicates diabetes.
4. A1C Test
- When it’s used: Provides your average blood sugar over the past 2–3 months by measuring the percentage of red blood cells with glucose attached.
- Diagnostic ranges:
- Normal: Below 5.7%
- Prediabetes: 5.7–6.4%
- Diabetes: 6.5% or higher
- Management targets: Many healthcare professionals recommend keeping A1C below 7% for most adults with diabetes, but this is not a one-size-fits-all goal. Your provider may adjust targets depending on your age, other health conditions, or risk of complications.
Normal Ranges Chart & Diagnostic Thresholds
Understanding your numbers starts with knowing whether a test is being used for diagnosis or for management. The cutoffs used to diagnose diabetes are not always the same as the target ranges set by healthcare professionals for people with diabetes.
Diagnostic Ranges
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Fasting plasma glucose (FPG) | 70-99 mg/dL | 100-125 mg/dL | 126 mg/dL or higher |
| Oral glucose tolerance test (OGTT, 2 hours) | Below 140 mg/dL | 140–199 mg/dL | 200 mg/dL or higher |
| Random plasma glucose | Varies with meals, generally <140 mg/dL | 200 mg/dL or higher with symptoms | |
| A1C test | Below 5.7% | 5.7%–6.4% | 6.5% or higher |
Management Targets (For People with Diabetes)
| Time of Check | Recommended Target Range | Notes |
|---|---|---|
| Before meals (fasting/pre-meal) | 80–130 mg/dL | May be individualized based on age or health conditions |
| 2 hours after meals | Below 180 mg/dL | Some individuals may benefit from stricter or looser targets |
| A1C test (long-term average) | Typically <7% | Providers may adjust based on risk of lows, age, or other health conditions |
Risks of High & Low Blood Sugar
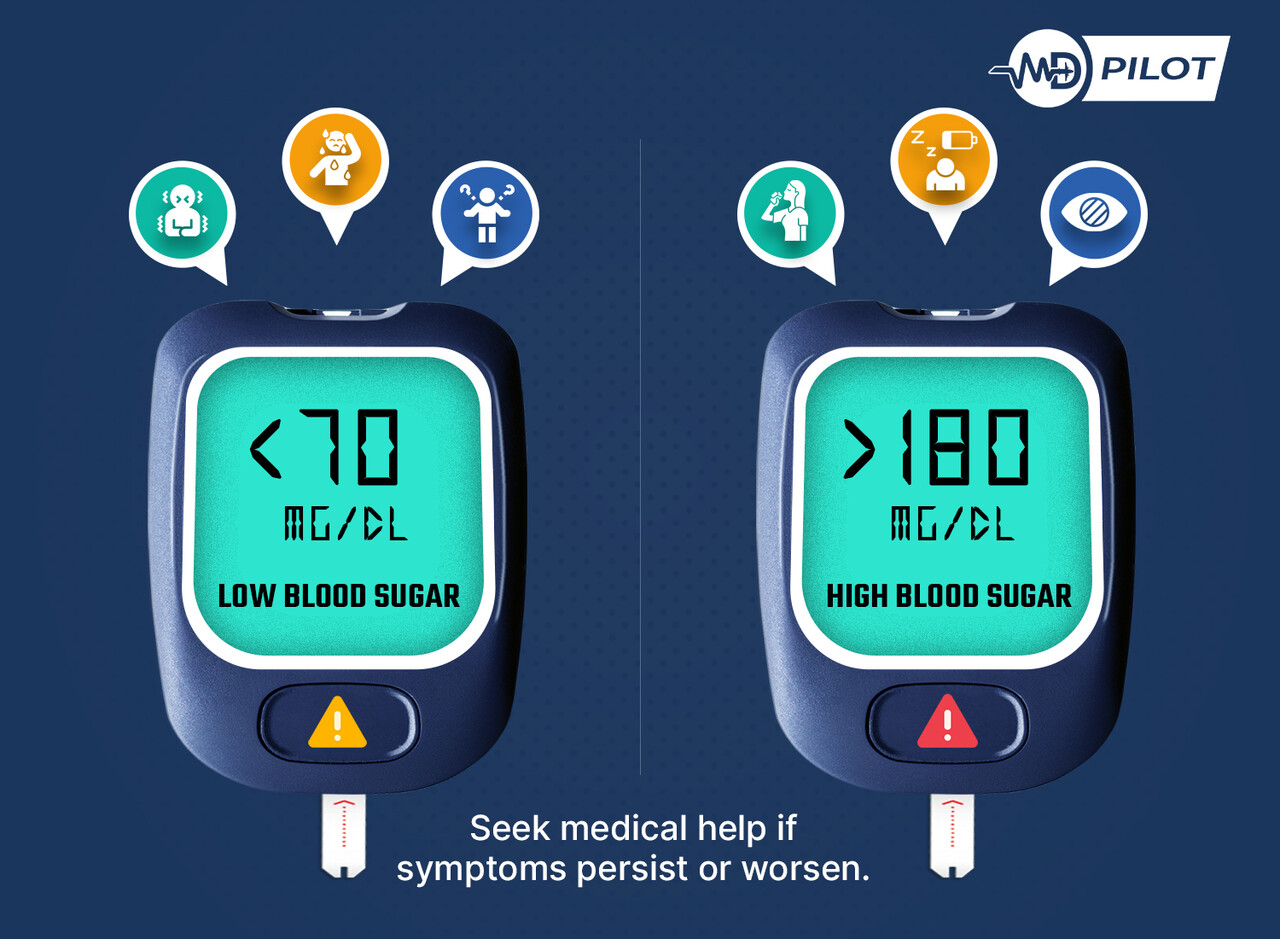
Your blood sugar levels naturally rise and fall throughout the time of day, but persistent highs or repeated lows can signal a problem. Understanding these risks helps you act sooner and work with healthcare professionals on the right management plan.
1. Low Blood Sugar (Hypoglycemia)
Hypoglycemia happens when blood glucose drops below 70 mg/dL. Common signs and symptoms include shakiness, sweating, irritability, dizziness, or blurred vision. If levels fall close to 55 mg/dL, more severe effects like confusion, seizures, or loss of consciousness may occur (ADA 2025).
Low blood sugar is often linked to medications like insulin or sulfonylureas, skipping meals, or unplanned physical activity. Treating lows quickly with fast-acting carbs such as glucose tablets, juice, or regular soda is critical.
2. High Blood Sugar (Hyperglycemia)
Hyperglycemia occurs when blood glucose levels remain above the recommended target range. Short-term effects include thirst, frequent urination, and fatigue. If left untreated, it can lead to diabetic ketoacidosis (DKA) in type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in type 2 diabetes — both medical emergencies (CDC).
Long-term, consistent high blood sugar increases the risk of complications affecting the eyes, kidneys, nerves, and heart. That’s why adults with diabetes are encouraged to monitor regularly and aim to keep levels within their agreed-upon target range.
How to Keep Blood Sugar Levels in a Healthy Range (Management Plan)
Managing blood sugar levels isn’t about a single habit; it’s the result of consistent daily choices, smart use of technology, and guidance from medical professionals. A strong management plan can help reduce the risk of both highs and lows while improving overall health.
1. Nutrition & Meal Planning
- Focus on balanced meals that include fiber, lean protein, and healthy fats.
- Keep an eye on carbohydrate intake, since carbs most directly affect blood glucose levels.
- Eating at consistent times can help avoid sudden drops or spikes.
- Limit processed foods and added sugars to reduce the chance of high blood sugar.
2. Exercise & Physical Activity
- Aim for at least 150 minutes of moderate exercise per week, such as walking, cycling, or swimming.
- Be mindful that activity lowers blood sugar; check before, during, and after workouts to prevent unexpected lows.
- When you exercise, always carry a quick source of carbohydrates, such as juice or glucose tablets, to stabilize blood sugar if it drops.
3. Glucose Monitoring & Technology
- Regular blood sugar tests help identify trends across the time of day.
- Many people now use continuous glucose monitoring (CGM) systems for real-time insights and predictive alerts.
- Discuss monitoring frequency with your provider to match your health conditions and medication use.
4. Lifestyle Factors
- Sleep: Poor sleep can raise insulin resistance and make it harder to maintain stable blood sugar levels.
- Stress: Stress hormones (like cortisol) may elevate glucose. Try mindfulness, deep breathing, or light activity to reduce impact.
- Hydration: Drinking water regularly supports kidney function and helps regulate glucose balance.
5. Partnering With Healthcare Professionals
- A personalized management plan works best. Your provider may adjust your target range, medications, or diet depending on your age, risk of complications, or other health conditions.
- Routine A1C tests help track progress toward long-term goals.
- For people with diabetes, working closely with healthcare professionals ensures you’re not just lowering numbers but protecting your overall health.
Frequently Asked Questions (FAQs)
Managing blood sugar is rarely straightforward, and readers often have lingering questions even after learning the basics. These answers address real-world concerns and common misunderstandings.
Blood sugar naturally shifts depending on the time of day, meals, activity, stress, and sleep. A morning rise, called the “dawn phenomenon,” is common in people with diabetes. Regular glucose monitoring helps spot patterns.
Not always. A reading of 140 mg/dL two hours after eating is considered the upper end of normal for adults without diabetes. For adults with diabetes, the ADA recommends keeping post-meal levels below 180 mg/dL, though individual management plans may differ.
An A1C test reflects your average blood sugar over 2–3 months, while a single blood sugar test measures one point in time. Both are important: A1C tracks long-term stability, while daily monitoring helps manage immediate highs and lows.
Yes. Certain health conditions — including hormonal disorders, kidney disease, and infections — can raise or lower blood glucose levels. That’s why working with healthcare professionals is key to tailoring your management plan.
Mild spikes after meals can be managed with light activity, hydration, and balanced food choices. For persistent high blood sugar, or if readings exceed 200 mg/dL, you should follow your provider’s guidance — never self-adjust medications without medical advice.
Mastering Your Blood Sugar Starts Here
A chart of normal blood sugar levels is more than a reference guide — it’s a roadmap for protecting your long-term health.
Knowing your numbers is only the beginning. The real impact comes from using that knowledge to shape daily choices, from meal planning to exercise, stress control, and consistent glucose monitoring. With the right management plan in place, you can reduce risks, prevent complications, and build a stronger foundation for the future.
At MD Pilot, our goal is to turn medical research into practical steps you can use today. Explore our in-depth guides on diabetes management, meal strategies, and monitoring tools, or subscribe to our Weekly Health Intel for evidence-based insights delivered straight to your inbox. Because when you understand your numbers, you can turn them into daily choices that protect your health and shape your future.
List of References:
- American Diabetes Association. Standards of Care in Diabetes—2025. Diabetes Care, 48(Supplement 1). https://diabetesjournals.org/care/issue/48/Supplement_1
- Centers for Disease Control and Prevention (CDC). Diabetes Testing and Diagnosis. https://www.cdc.gov/diabetes/diabetes-testing/index.html
- Mayo Clinic. A1C Test: What It Is and Why It’s Done.
https://www.mayoclinic.org/tests-procedures/a1c-test/about/pac-20384643 - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes & Prediabetes Tests.
https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/diabetes/diabetes-prediabetes
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




