Table Of Contents
-
Key Highlights:
-
What Is Hypoglycemia & When Does It Become Dangerous?
- The Neuroglycopenic Process: Can Low Blood Sugar Cause Seizures?
- Who Is At Risk Of Hypoglycemic Seizures?
-
How To Prevent Seizures From Low Blood Sugar
-
FAQs About Low Blood Sugar Causing Seizures
-
Unlock Life-Saving Hypoglycemia Insights Through MD Pilot
-
References
While low blood sugar (hypoglycaemia) is often brushed off as a harmless “energy dip,” this may not always be the case.
The condition could lead to mild symptoms such as shakiness or fatigue, and in rare but serious situations, very low blood sugar can disrupt brain function enough to trigger seizures. This makes it essential to understand the risks associated with this condition and to address a key question many readers may have: Can low blood sugar cause seizures?
Research shows that about 5% of people with severe hypoglycaemia experience seizures. Surprisingly, however, the blood glucose levels of patients with and without seizures may not differ significantly. Hence, seizures linked to hypoglycaemia, though rare, are potentially life-threatening. Besides people with diabetes, infants, older adults, and anyone with unstable glucose regulation may be struck by them.
This article is designed as a practical guide on seizures related to low blood sugar. In the following sections, we will explain what happens inside the body when blood sugar drops, how to detect and treat these episodes, and prevention tips. With that in mind, let us get started.
Key Highlights:
- Low blood sugar may be more than an “energy dip” and, if left unchecked, can trigger seizures and even long-term brain damage.
- Seizures from hypoglycemia are rare but dangerous, affecting not only people with diabetes but also infants, older adults, and those with unstable glucose control.
- Early warning signs like shaking, confusion, or slurred speech often provide a critical window to act before a seizure occurs.
- Prevention requires a layered approach, including regular monitoring, medication management, emergency preparedness, and lifestyle adjustments.
What Is Hypoglycemia & When Does It Become Dangerous?
Hypoglycemia is when the body’s blood sugar level dips lower than normal. Warning signs usually emerge when readings fall under 70 mg/dL. This drop often results from factors such as excessive diabetes medications, skipped meals, or an imbalance between insulin doses and food intake, all of which heighten vulnerability to low glucose episodes.

Healthy blood sugar levels support normal brain function. For adults without diabetes, blood sugar after not eating for at least eight hours usually falls between 72–99 mg/dL and should remain under 140 mg/dL two hours after a meal. For those living with diabetes, the American Diabetes Association advises targets of 70–130 mg/dL before meals and under 180 mg/dL afterward.
However, levels below 55 mg/dL are considered dangerously low and linked with a three-times greater risk of mortality. Individuals with type 1 diabetes experience symptoms of low blood sugar about twice per week on average, underscoring the need for vigilance. To simplify, hypoglycemia severity can be grouped as:
| Hypoglycemia Severity | Blood Sugar Level Range | Health Risk(s) |
|---|---|---|
| Mild | 56–70 mg/dL | Initial Warning Signs |
| Severe | Below 55 mg/dL | Heightened Seizure Risk |
| Critical | Below 40 mg/dL | Life-Threatening Emergency |
The Neuroglycopenic Process: Can Low Blood Sugar Cause Seizures?
The human brain consumes nearly 20-25% of the body’s glucose at any time, and this steady supply is crucial for normal function. Without enough glucose, neurons fail to operate correctly. This shortage leads to neuroglycopenic symptoms (such as headaches, blurred vision, poor coordination, etc.) and eventually causes seizures. Here’s what happens in the brain during hypoglycemia:
1. Energy Supply Is Cut
Think of your neurons as tiny power plants. They need a constant sugar stream to make energy (Adenosine Triphosphate or ATP). When blood sugar drops too far, energy production slows down, and brain cells misfire. This weakened state is one primary reason why severe hypoglycemia can cause seizures.
2. Neurotransmitter Imbalance
Your brain also depends on a delicate chemical balance to stay calm. During hypoglycemia, the “brakes” (inhibitory GABA signals) get weaker while the “gas pedal” (excitatory glutamate) gets stronger. This chemical shift overstimulates nerve cells, increasing the chance that low blood sugar causes seizures during a sharp glucose drop.
3. Ion Channel Dysfunction & Neuronal Excitability
Every brain cell uses a tiny pump (the sodium–potassium pump) to keep electrical signals balanced, like a battery holding its charge. When glucose levels fall, it causes instability. The cell’s charge starts leaking, making nerve cells more excitable. This unstable state increases the likelihood of low blood glucose levels causing seizures by triggering uncontrolled electrical surges.
4. Structural Or Longer-term Damage In Repeated/Prolonged Episodes
Recurrent or prolonged hypoglycemia does more than trigger short-term seizures. It can cause lasting structural brain damage over time. For instance, newborns with repeated hypoglycemia may develop brain lesions that increase the risk of chronic seizures later on. This demonstrates why early detection and prevention are essential to avoid lasting harm from hypoglycemia.
How Hypoglycemia Unawareness Increases Seizure Risk
Some of the most serious low blood sugar episodes appear without obvious warning. Repeated hypoglycemia can train the body to ignore its usual alerts, such as sweating or shakiness. This loss of early cues, called hypoglycemia unawareness, raises the risk of critical glucose drops and sparks the question: Can low blood sugar cause seizures if left unnoticed?
Seizures or even coma can be the first sign of trouble. In such cases, routine testing and preventive habits are vital for anyone prone to frequent lows. By preventing low readings for several weeks and tracking glucose closely, many individuals regain sensitivity to the early warning symptoms. This restored awareness gives them a crucial chance to act before blood sugar reaches harmful levels.
Who Is At Risk Of Hypoglycemic Seizures?
While anyone can experience low blood sugar, certain groups face higher risks due to metabolic, genetic, or lifestyle factors. Identifying these factors helps clarify why some individuals are more likely to experience severe symptoms and directly addresses concerns about low blood sugar causing seizures.
1. Neonates & Infants
Newborns and infants are particularly vulnerable due to immature metabolic regulation, low glycogen stores, and potential perinatal stress. These factors make maintaining stable blood sugar challenging. Consequently, if glucose drops too low, their delicate system may trigger neurological events, so close monitoring is essential.
2. People With Type 2 Or Type 1 Diabetes
Individuals with diabetes, especially those on insulin or other diabetes medications, should ensure their monitoring routine measures blood sugar frequently to avoid dangerous lows. Sudden drops in blood sugar may occur despite careful management. Therefore, regular monitoring and prompt treatment are critical, as untreated hypoglycemia could occasionally escalate into seizures.
3. Individuals With Alcohol-Related Diseases
Chronic alcohol consumption can impair liver glucose production and metabolism. Combined with inadequate nutrition, this may create rapid drops in blood sugar. As a result, these individuals are at increased risk of severe hypoglycemic episodes, and in rare cases, seizures may occur if untreated. Recognizing this link is essential for timely intervention.
4. Those With Metabolic Or Genetic Disorders
Conditions such as hyperinsulinism or inborn errors of metabolism, like GLUT1 deficiency, disrupt glucose production or transport. These impairments make it difficult for the body to maintain normal blood sugar levels. Consequently, hypoglycemia may occasionally lead to neurological complications such as seizures if left unmanaged.
5. Individuals With Other Systemic Illnesses Or Eating Disorders
Systemic conditions such as liver or kidney failure, sepsis, or chronic illnesses can compromise glucose regulation. Similarly, individuals with eating disorders may experience frequent low blood sugar due to insufficient intake. In both cases, there’s a clear risk of hypoglycemic episodes, and in uncommon instances, seizures may develop without timely intervention.
Common Symptoms Leading Up To A Hypoglycemic Seizure
Recognizing the warning signs of impending low blood sugar seizures can be life-saving. Unlike epileptic seizures that often occur without warning, hypoglycemic seizures typically progress through distinct stages, giving you critical time to intervene. Here are the symptoms of low blood sugar leading up to a hypoglycemic seizure:
| Signs | Early Hypoglycemia Levels Warnings | Severe Hypoglycemic Symptoms | Pre-Seizure Warning |
|---|---|---|---|
| Physical Symptoms | Shaking, sweating, hunger pangs | Unsteady gait, slurred speech, muscle weakness, temporary blindness | Involuntary jerking movements, especially in facial muscles |
| Neurological Symptoms | Dizziness, blurred vision, tingling in lips or fingers | Confusion, difficulty speaking, disorientation, visual hallucinations | Difficulty staying awake or responding to verbal commands |
| Behavioral Changes | Irritability, anxiety, restlessness, difficulty concentrating | Inappropriate behavior, personality changes | Fixed gaze, unresponsiveness to surroundings, purposeless movements like lip smacking |
When To Call Emergency Services
Even with excellent preparation, emergencies can still happen. Some scenarios demand immediate action. Call 911 without delay if a hypoglycemic seizure is suspected, especially when the episode lasts longer than five minutes, which may signal status epilepticus, a life-threatening condition that needs urgent medical intervention.
Multiple seizures occurring back-to-back also indicate severe hypoglycemia that requires rapid medical attention. If the person remains unresponsive after the seizure stops and glucagon has been given, emergency services should be contacted immediately. Waiting to see if symptoms improve can significantly increase the risk of complications or lasting harm in these situations.
Breathing difficulties, blue lips or fingernails, or any severe injury such as head trauma during the seizure also warrant urgent evaluation. Finally, treat any first-time seizure in someone without a history of seizures as an emergency. Prompt recognition and calling emergency services can dramatically improve outcomes and prevent further danger.
How To Prevent Seizures From Low Blood Sugar
Preventing hypoglycemia is a multi-layered approach. Monitoring, emergency preparedness, medication management, lifestyle adjustments, and dietary planning create a safety net. Each strategy works in tandem to reduce the risk and severity of episodes, ensuring daily glucose stability and lowering the likelihood of low blood sugar causing seizures.
1. Frequent Monitoring
The best defense against hypoglycemia is prevention. Continuous glucose monitors (CGMs) or at-home test kits measure blood glucose at set intervals. Additionally, hybrid closed-loop systems can be leveraged to automatically adjust insulin while using predictive low glucose suspension and smart insulin pens to help prevent dangerous drops. Even mobile apps integrate all diabetes management information for better control.
2. Emergency Detection & Alert Systems
Even with monitoring, unexpected lows can happen. Utilize wearable seizure-detection devices to identify convulsive movements and connect with smart home systems for automated emergency responses. Remote monitoring services also notify professionals, and family alert systems ensure that caregivers are informed instantly. These layered safety measures minimize delays in intervention, crucial given that low blood sugar sometimes leads to seizures.
3. Medication Management
Collaborate with your healthcare team to optimize insulin dosing and maintain consistent timing. Adjust doses for exercise, schedule changes, or illness. For non-insulin medications, especially sulfonylureas, coordinate meals, understand drug interactions, and review your regimen periodically. Remember that proper medication management is a key preventive measure for severe hypoglycemia events.
4. Sleep & Stress Regulation
Sleep and stress impact glucose stability. Maintain regular sleep and wake times to aim for bedtime glucose levels between 120–180 mg/dL. Keep your CGM and glucagon kit accessible. Furthermore, educate partners on hypoglycemia signs. Manage stress with relaxation techniques, strong support networks, or professional counseling to reduce the risk of unpredictability in glucose fluctuations and improve overall health.
5. Exercise & Activity Planning
Before starting any activity, check your blood sugar. If it is below 100 mg/dL, consume 15 grams of carbohydrates to stabilize glucose levels first. Adjust insulin doses based on exercise intensity, stay hydrated, and monitor glucose continuously during longer workouts. Always carry emergency glucose, use a buddy system, and monitor for up to 24 hours to prevent delayed hypoglycemic events.
6. Dietary Strategies
Consistent meal timing and balanced macronutrients stabilize glucose levels and help prevent complications. Carry fast-acting 15 grams of carbohydrates for emergencies, fuel with complex carbs and protein before bedtime or exercise, and pack extra snacks when traveling. Avoid alcohol on an empty stomach. These dietary habits are simple yet effective ways to reduce the chance of low blood sugar causing seizures.
FAQs About Low Blood Sugar Causing Seizures
You likely have questions now that we have examined how low blood sugar impacts the brain and triggers seizures. The following FAQs provide clear guidance on recognizing symptoms, responding safely, and preventing complications from hypoglycemia-induced seizures.
Epileptic seizures result from abnormal electrical activity in the brain and are not necessarily triggered by glucose levels. In contrast, hypoglycemia-induced seizures occur directly because of low blood sugar and often present gradual warning signs. Diagnostic tools, such as EEG combined with glucose measurement, are essential to differentiate between the two conditions.
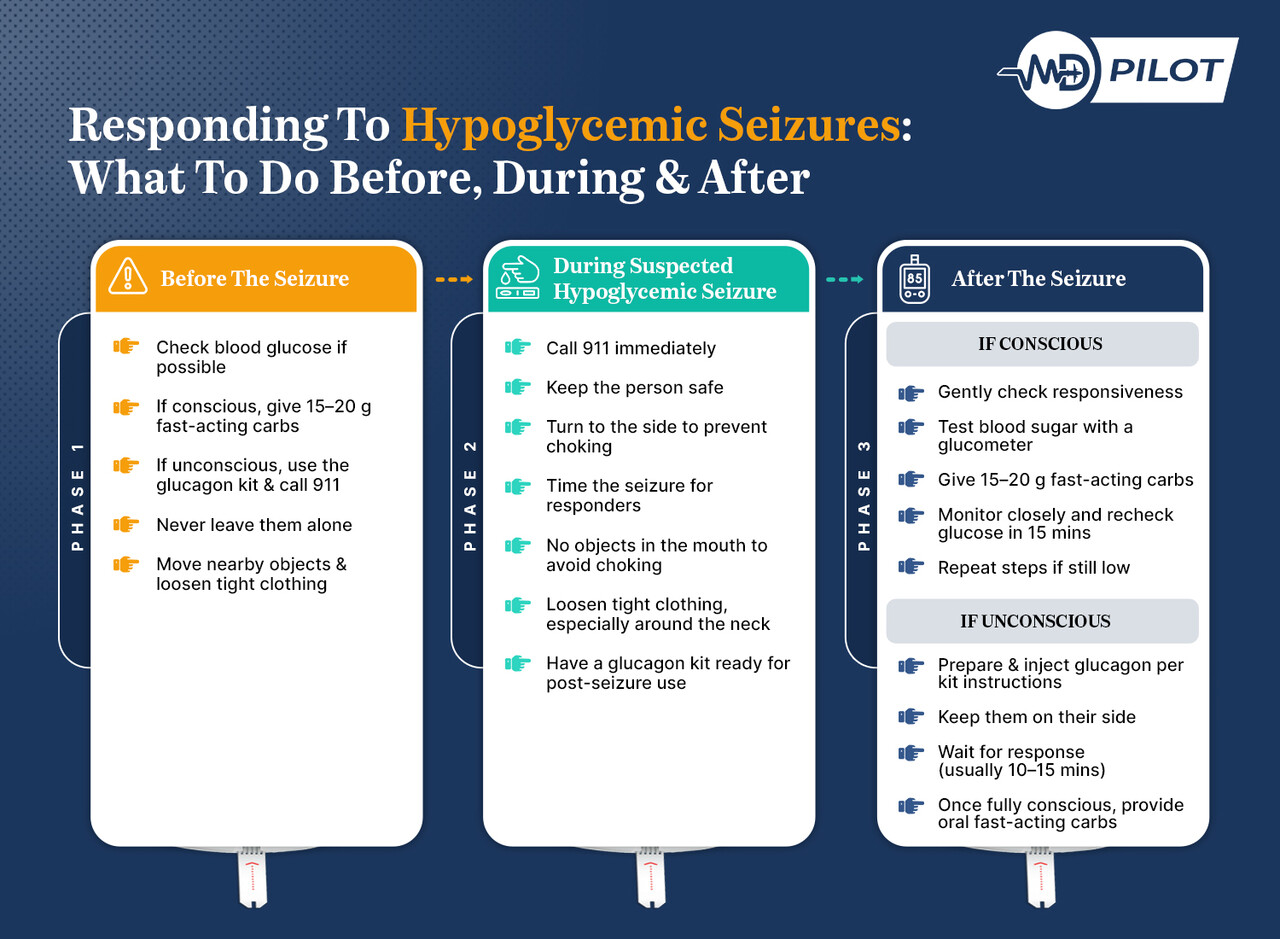
Immediate action is critical. Call 911, ensure the person and the surrounding area are safe, and note the seizure duration for emergency responders. Do not place anything in their mouth. Once the seizure stops, administer glucagon if available and continue monitoring until professional help arrives.
Nocturnal hypoglycemic seizures occur during sleep and are particularly dangerous because symptoms often go unnoticed. Without intervention, glucose can drop to critically low levels. Continuous glucose monitors with nighttime alarms, maintaining bedtime glucose targets between 120–180 mg/dL, and adjusting diet or medication can significantly reduce the risk.
Yes, prolonged or severe hypoglycemic seizures can lead to lasting brain injury. The brain relies entirely on glucose, and extended periods below 40 mg/dL may cause memory impairment, cognitive decline, personality changes, or motor dysfunction. However, prompt glucose administration often prevents permanent damage, highlighting the importance of rapid intervention.
Recovery largely depends on seizure duration, glucose levels, and speed of treatment. Most individuals regain full cognitive and physical function after timely correction, but temporary confusion may last hours or days. Repeated severe episodes increase the risk of long-term cognitive and cardiovascular complications, emphasizing proactive diabetes management and seizure prevention strategies.
Diabetic seizures can occur due to extreme fluctuations in blood glucose. Severe low blood sugar (hypoglycemia) deprives the brain of fuel, while extreme high blood sugar (hyperglycemia) causes metabolic imbalances and electrolyte shifts that may also trigger seizures. Managing blood glucose levels within target ranges and regular monitoring considerably lowers these risks for people with diabetes.
Unlock Life-Saving Hypoglycemia Insights Through MD Pilot
Seizures caused by low blood sugar are serious yet largely preventable. Although they don’t happen every day, the consequences can be severe, ranging from brain injury and long-term neurological effects to death in extreme cases. Therefore, it is crucial to identify who is at risk, recognize warning signs, and implement early monitoring and rescue strategies.
At MD Pilot, we aim to empower you with expert-verified medical insights, decision-making tools, and free resources. Whether you manage diabetes, care for infants, or handle metabolic disorders, our resources, including the Glucose to HbA1c Estimator and Blood Sugar Level Interpreter, provide guidance, clarity, and confidence. They ensure you and your caregivers are never caught off guard by hypoglycemia.
By staying informed and proactive, you can dramatically reduce the risk of low blood sugar–related seizures. Our tools, such as the 7-Day Blood Sugar Tracker and Trend Analyzer, are designed to help you recognise patterns, take preventive steps early, and protect your health and peace of mind.
References
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/hypoglycemia-low-blood-sugar
- https://www.webmd.com/diabetes/how-sugar-affects-diabetes
- https://www.cdc.gov/diabetes/treatment/treatment-low-blood-sugar-hypoglycemia.html
- https://diabetes.org/living-with-diabetes/hypoglycemia-low-blood-glucose/severe
- https://www.cdc.gov/diabetes/treatment/treatment-low-blood-sugar-hypoglycemia.html
- https://www.mdpi.com/2077-0383/12/7/2580
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




