Table Of Contents
-
Key Highlights
- How Cold Exposure Influences Blood Sugar and Insulin Sensitivity
- The Science Behind Cold Showers and Glucose Metabolism
- Practical Benefits and Risks of Cold Showers for Diabetes Management
- Cold Showers vs. Other Cold Therapies: What You Need to Know
- Understanding the Research Limitations
-
Frequently Asked Questions About Cold Showers and Blood Sugar
-
Conclusion: Cold Showers as Part of Your Blood Sugar Strategy
-
References
If you’ve heard about cold showers helping with blood sugar control, you’re not imagining things. Recent research suggests that voluntary cold exposure—including cold showers—may actually improve insulin sensitivity and glucose metabolism. While this might sound like wellness hype, the science behind cold therapy and blood sugar regulation is surprisingly robust.
For people with type 2 diabetes or prediabetes, managing blood sugar levels often feels like a full-time job. Medications, diet changes, and exercise routines are the standard tools. But what if something as simple as turning down your shower temperature could complement these efforts? Research published in 2021 examined cold exposure as a therapeutic strategy for obesity and type 2 diabetes, revealing fascinating metabolic benefits.
This article breaks down the current research on cold showers and blood sugar levels, explains the biological mechanisms at work, and helps you understand whether this practice might benefit your diabetes management plan. We’ll separate the science from the hype and give you practical, evidence-based guidance.
Key Highlights
- Cold exposure triggers metabolic benefits: Cold showers can increase energy expenditure and improve insulin sensitivity through mechanisms like shivering thermogenesis and brown adipose tissue activation.
- Research shows promise for type 2 diabetes: Studies indicate that repeated cold exposure may reduce fasting glucose and insulin levels in people with type 2 diabetes.
- Hormonal effects matter: Cold exposure stimulates adiponectin production—a hormone that protects against insulin resistance and improves glucose metabolism.
- Shivering burns glucose: The metabolic benefits partly stem from increased glucose uptake by muscles during shivering, which can raise metabolic rate up to 5 times basal levels.
- Safety is paramount: Cold shock response can stress the cardiovascular system, especially for people with heart conditions or diabetes—medical guidance is essential before starting.
- Not a medication replacement: Cold showers may complement lifestyle interventions but cannot replace prescribed diabetes treatments or proper blood sugar management.
- More research needed: While promising, long-term studies specifically on cold showers (versus ice baths or immersion) for blood sugar control remain limited.
How Cold Exposure Influences Blood Sugar and Insulin Sensitivity
The connection between cold exposure and blood sugar regulation centers on your body’s adaptive response to cold stress. When you’re exposed to cold temperatures, your body activates several physiological mechanisms to maintain core temperature—and these mechanisms have unexpected metabolic benefits.
Shivering Thermogenesis: Your Body's Natural Furnace
When cold water hits your skin, your muscles contract rapidly in what we call shivering. This isn’t just about keeping warm—it’s a metabolic powerhouse. Research by Ivanova and colleagues found that shivering thermogenesis can increase your metabolic rate up to five times your resting level. During this process, your muscles consume significant amounts of glucose for fuel, effectively lowering blood sugar levels.
Think of shivering as an unintentional workout. Your muscles are contracting repeatedly, burning through glucose stores to generate heat. For someone with type 2 diabetes management challenges, this increased glucose uptake happens without requiring insulin—which is particularly valuable when insulin resistance is an issue.
Timeline: When Cold Exposure Effects Occur
0-15 Minutes
Immediate Effects:
• Cold shock response activated
• Heart rate ↑ 15-30%
• Blood pressure ↑ 10-20 mmHg
• Shivering begins
• Glucose uptake increases in muscles
15-60 Minutes
Short-Term Effects:
• BAT activation peaks
• Norepinephrine surge
• Metabolic rate ↑ 350%
• Blood sugar drops 10-15 mg/dL
• Thermogenesis continues
1-24 Hours
Post-Exposure:
• Elevated metabolic rate persists
• Improved insulin sensitivity
• Adiponectin levels rise
• Anti-inflammatory markers ↑
• Enhanced fat oxidation
4-8 Weeks
Long-Term Adaptations:
• Cold habituation complete
• BAT volume increases
• Fasting glucose ↓ 5-10%
• HbA1c improvement
• Sustained insulin sensitivity
Visual Guide: The intensity and duration of cold exposure determines the magnitude of these effects. Consistency (3-5x/week) produces the strongest long-term adaptations.
Brown Adipose Tissue Activation
Here’s where things get interesting. Humans have two types of fat: white adipose tissue (regular fat that stores energy) and brown adipose tissue (BAT), which burns energy to produce heat. Cold exposure activates BAT through a process called non-shivering thermogenesis.
A comprehensive 2022 review published in PMC highlighted that brown fat activation improves glucose metabolism and insulin sensitivity. While BAT accounts for roughly 20 calories per day at rest, cold acclimation can significantly increase this thermogenic activity. The beauty of BAT is that it pulls glucose and fatty acids from your bloodstream to fuel heat production—effectively acting as a natural blood sugar regulator.
Hormonal Changes That Support Glucose Control
Cold exposure doesn’t just affect muscles and fat—it triggers a cascade of hormonal responses. One key player is adiponectin, a hormone that enhances insulin sensitivity and has anti-inflammatory properties. Studies have shown that regular cold exposure increases adiponectin levels, which correlates with better glucose metabolism.
Additionally, cold exposure stimulates norepinephrine release, which not only activates brown fat but also influences how your body handles glucose. This hormonal shift can improve your cells’ responsiveness to insulin—addressing one of the core problems in type 2 diabetes.
| Stage | Physiological Response | Blood Sugar Effect |
|---|---|---|
| 1. Cold Exposure | Cold water contacts skin, activating thermoreceptors | Initial trigger - no immediate effect |
| 2. Shivering | Rapid muscle contractions generate heat (metabolic rate ↑5x) | ↓ Glucose consumed by muscles for energy |
| 3. Brown Fat Activation | BAT burns glucose + fatty acids via non-shivering thermogenesis | ↓ Glucose uptake from bloodstream |
| 4. Hormonal Response | Release of norepinephrine and adiponectin increases | ↑ Insulin sensitivity improvement |
| 5. Net Result | Enhanced metabolic flexibility and glucose regulation | ✓ Better blood sugar control |
The Science Behind Cold Showers and Glucose Metabolism
While ice baths and cold water immersion have received more scientific attention, cold showers represent a more accessible form of cold therapy. Understanding how they differ from other cold exposure methods—and what the research specifically shows—helps set realistic expectations.
Cold Showers vs. Other Cold Therapies
Cold showers typically involve water temperatures between 50-70°F (10-21°C) for 5-10 minutes. In contrast, cold water immersion or ice baths use temperatures around 50°F (10°C) or colder with full body submersion for 10-20 minutes. Case Western Reserve University’s analysis points out that ice baths create more intense cold exposure, triggering stronger metabolic responses.
The intensity difference matters for blood sugar effects. Ice baths produce more dramatic shivering and BAT activation, potentially offering greater glucose metabolism benefits. However, cold showers are safer for most people, easier to incorporate into daily routines, and still trigger meaningful metabolic responses—just at a lower magnitude.
What Research Shows About Cold Showers Specifically
Direct research on cold showers and blood sugar is limited compared to cold immersion studies. However, the 2022 PMC review on voluntary cold water exposure found that repeated cold exposure—even milder forms—can improve insulin sensitivity and reduce fasting glucose levels over time.
One notable finding: consistency matters more than intensity. Regular cold shower practice (3-5 times per week) showed metabolic adaptations in study participants, including improved glucose tolerance. The body essentially becomes more efficient at managing cold stress, and these adaptations carry metabolic benefits even when you’re not cold.
The Cold Stress Response
When you first step into a cold shower, your body undergoes what’s called the cold shock response—rapid breathing, increased heart rate, and elevated blood pressure. While this sounds alarming, it’s a normal physiological reaction. Over weeks of regular exposure, this response moderates as your body adapts.
This adaptation process is called cold habituation, and it’s crucial for the glucose metabolism benefits. Your nervous system becomes more efficient at regulating the stress response, your BAT becomes more active at baseline, and your metabolic flexibility—your body’s ability to switch between fuel sources—improves. All of these factors contribute to better blood sugar control.
Cold Adaptation Progression Chart
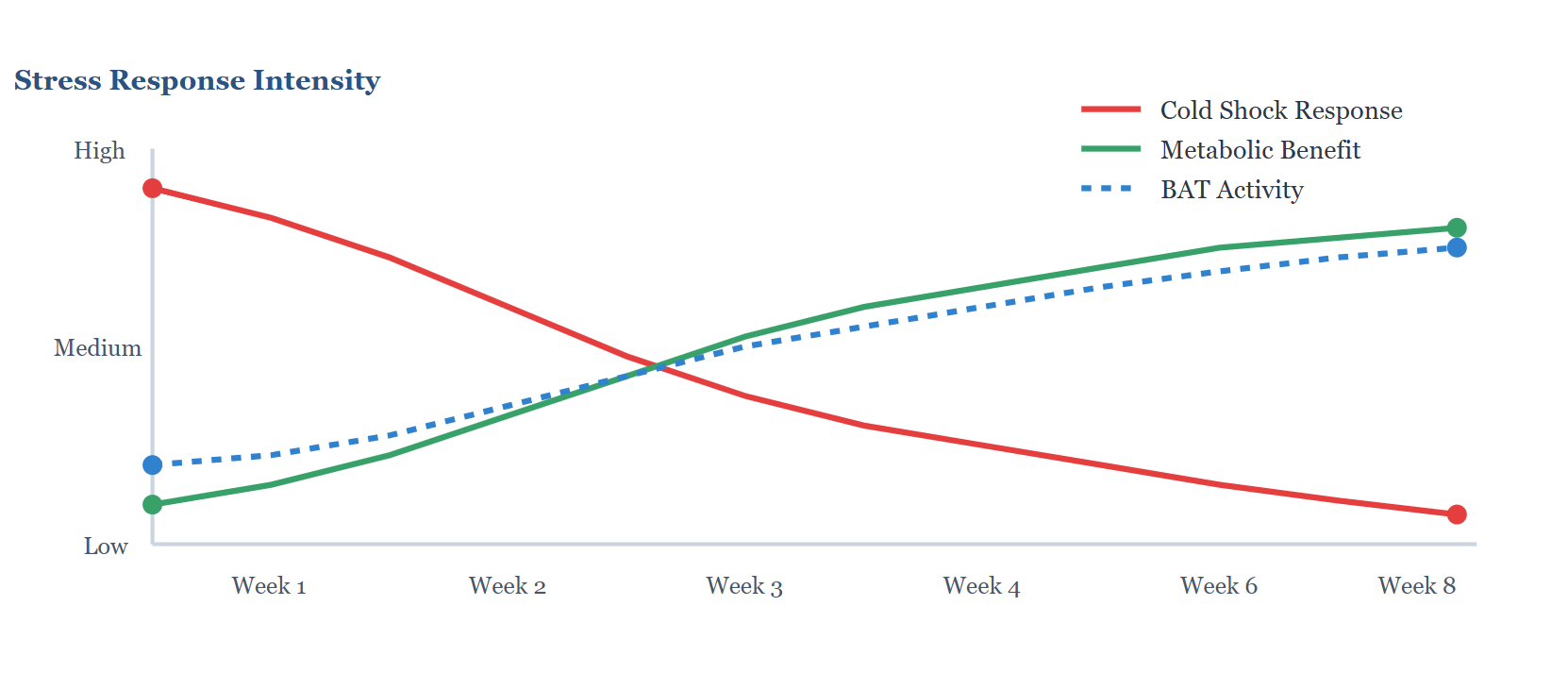
 Key Insight:
Key Insight:
As your body adapts to regular cold exposure over 4-8 weeks, the initial cardiovascular stress (red line) decreases significantly while metabolic benefits (green line) and brown fat activity (blue line) continue to improve. This adaptation makes cold showers safer and more effective over time.
Practical Benefits and Risks of Cold Showers for Diabetes Management
Before you turn your shower dial all the way to cold, it’s essential to understand both the potential benefits and significant risks—especially if you have diabetes or cardiovascular issues.
Potential Benefits Beyond Blood Sugar
The glucose metabolism improvements from cold showers come with additional health benefits that matter for diabetes management:
- Weight management support: Increased metabolic rate and brown fat activation can contribute to modest fat loss over time, which improves insulin sensitivity.
- Inflammation reduction: Cold exposure has anti-inflammatory effects, and chronic inflammation is a key factor in insulin resistance.
- Improved circulation: Regular cold exposure strengthens blood vessels, which is particularly important for people with diabetes who face higher cardiovascular risks.
- Mental resilience: The stress adaptation from cold exposure may improve your ability to handle other stressors that affect blood sugar, like anxiety or poor sleep.
Cardiovascular and Safety Risks
Here’s the critical part: cold exposure stresses your cardiovascular system. Harvard Health Publishing warns that the cold shock response causes rapid increases in heart rate and blood pressure, which can trigger arrhythmias or cardiac events in vulnerable individuals.
People with diabetes already face elevated cardiovascular risks. Adding cold stress without medical guidance could be dangerous. The CDC emphasizes that people with diabetes need to be especially careful with cold exposure, as it can affect blood circulation and potentially mask symptoms of hypoglycemia.
Additional safety concerns include:
- Risk of hypothermia with prolonged exposure
- Difficulty detecting low blood sugar while cold (cold can mimic hypoglycemia symptoms)
- Potential for nerve damage in people with diabetic neuropathy
- Increased fall risk if you experience dizziness from the cold shock response
Guidelines for Safe Cold Shower Practice
If your healthcare provider approves cold shower therapy, follow these safety guidelines:
- Start gradually: Begin with 30 seconds of cold water at the end of your regular warm shower, then slowly increase duration over weeks.
- Check blood sugar before and after: Monitor how cold exposure affects your glucose levels, especially in the first few weeks.
- Never go in cold: Start with warm water and transition to cold—sudden cold shock is more dangerous.
- Keep it brief initially: Work up to 5-10 minutes maximum; more isn’t necessarily better.
- Stay safe: Use shower handles for stability, have someone nearby initially, and stop immediately if you feel dizzy, extremely cold, or experience chest discomfort.
- Avoid during illness or when feeling unwell: Cold stress adds to your body’s burden when you’re already fighting something.
- Warm up properly afterward: Dry off thoroughly and dress warmly to avoid prolonged cold exposure.
Safety Guidelines: Who Should/Shouldn't Try Cold Exposure
| Health Condition | Risk Level | Precautions | Recommendations |
|---|---|---|---|
| Cardiovascular Disease | HIGH | Cold shock can trigger arrhythmias, angina, or cardiac events | Avoid without cardiologist approval |
| Type 2 Diabetes (No Complications) | MODERATE | Monitor blood sugar closely; cold may mask hypoglycemia symptoms | Start gradually with doctor approval |
| Diabetic Neuropathy | HIGH | Impaired temperature sensation increases cold injury risk | High risk - avoid cold exposure |
| Hypertension (Controlled) | MODERATE | Cold raises blood pressure 10-20 mmHg temporarily | Consult doctor; brief exposure only |
| Prediabetes (Healthy Otherwise) | LOW | Start gradually; monitor for dizziness or discomfort | Good candidate with gradual approach |
| Elderly (65+) | HIGH | Reduced thermoregulation; higher fall risk; slower adaptation | Very brief exposure only with supervision |
| Raynaud's Syndrome | HIGH | Cold triggers severe vasoconstriction and circulation issues | Contraindicated - avoid entirely |
| Healthy Adults (18-50) | LOW | Start gradually; listen to body signals | Safe with gradual progression |
| Pregnancy | HIGH | Insufficient safety data; potential stress on fetus | Avoid - not worth potential risks |
 Important:
Important:
This table provides general guidance only. ALWAYS consult your healthcare provider before starting cold therapy, especially if you have any chronic health conditions. Individual risk varies based on overall health status, medication use, and specific complications.
Safe Cold Shower Progression Protocol (6-Week Plan)
| Week | Water Temperature | Duration | Frequency | What to Expect / Tips |
|---|---|---|---|---|
| 1 | Cool (65-70°F) | 30 seconds | 3x/week | Strong gasp reflex; rapid breathing. Focus on controlled breathing. End warm shower with brief cold. |
| 2 | Cool (60-65°F) | 1 minute | 3-4x/week | Breathing easier. Mild shivering begins. Check blood sugar before/after to track response. |
| 3 | Cold (55-60°F) | 2 minutes | 4x/week | Body adapting. Shivering more pronounced. Noticeable energy boost post-shower. |
| 4 | Cold (50-55°F) | 3-5 minutes | 4-5x/week | Cold shock response reduced. May notice improved insulin sensitivity. Stay present—don't push too hard. |
| 5 | Cold (50-55°F) | 5-7 minutes | 5x/week | Significant adaptation. Comfortable breathing. BAT activation increasing. Track fasting glucose trends. |
| 6 | Cold (50°F) | 8-10 minutes | 5x/week | Full adaptation achieved. Maintain this protocol. Review blood sugar logs with doctor for trends. |
 STOP IMMEDIATELY if you experience:
STOP IMMEDIATELY if you experience:
- Chest pain, pressure, or discomfort
- Severe dizziness, confusion, or numbness
- Uncontrollable shivering or inability to rewarm
- Signs of hypoglycemia (if diabetic)
- Irregular heartbeat or palpitations
Cold Showers vs. Other Cold Therapies: What You Need to Know
Understanding where cold showers fit in the spectrum of cold exposure therapies helps you make informed decisions about which approach might work for your situation.
Intensity and Effectiveness Comparison
Different cold therapies create different levels of metabolic stress and potential benefits:
| Method | Temperature | Duration | Intensity | Cost | Accessibility | Blood Sugar Impact | Safety Level |
|---|---|---|---|---|---|---|---|
| Cold Showers | 50-70°F (10-21°C) | 5-10 min | Mild-Moderate | Free | Excellent | Modest | High |
| Cold Water Immersion | 50-59°F (10-15°C) | 10-15 min | Moderate-High | $-$$ | Moderate | Moderate | Medium |
| Ice Baths | 40-50°F (4-10°C) | 10-20 min | High | $$ | Low | High | Lower |
| Cryotherapy | -200 to -300°F (-130 to -180°C) | 2-4 min | Very High | $$$ | Very Low | Moderate | Lowest |
Research strongly supports cold water immersion and ice baths for metabolic benefits, including improved insulin sensitivity and glucose control. Winter swimming studies have shown particularly impressive results, with regular swimmers demonstrating higher adiponectin levels and better metabolic markers compared to non-swimmers.
Accessibility and Practicality
Cold showers win on accessibility. You don’t need special equipment, gym memberships, or outdoor bodies of water. This makes them the most practical option for daily practice. While the metabolic effects might be less dramatic than ice baths, consistency trumps intensity for long-term health benefits.
For diabetes management specifically, the goal isn’t maximum cold stress—it’s sustainable practice that improves insulin sensitivity over time without excessive risk. Cold showers fit this criteria better than more extreme methods for most people.
Which Method Is Right for You?
Consider these factors when choosing your cold therapy approach:
- Current health status: If you have cardiovascular issues or complications from diabetes, cold showers are the safest starting point—if approved by your doctor.
- Cold tolerance: If you’re new to cold exposure, cold showers provide a gentler introduction than immersion.
- Consistency goals: Cold showers are easier to maintain daily compared to preparing ice baths.
- Desired intensity: Athletes and those seeking maximum metabolic benefits might progress to cold immersion after adapting to cold showers.
- Blood sugar control goals: For modest insulin sensitivity improvements, cold showers may suffice; for more significant metabolic changes, supervised cold immersion might be appropriate.
Understanding the Research Limitations
While the science on cold exposure and glucose metabolism is promising, it’s important to understand what we know—and what we don’t yet know—about cold showers specifically for blood sugar control.
What the Evidence Shows
Most robust research on cold exposure and diabetes comes from studies on cold water immersion, winter swimming, and controlled cold exposure in laboratory settings. The 2021 review by Ivanova and colleagues provides strong evidence that repeated cold exposure improves insulin sensitivity and glucose metabolism in people with type 2 diabetes.
However, these studies often involved more intense cold exposure than typical cold showers, or they measured acute responses rather than long-term adaptations. The mechanisms—shivering thermogenesis, BAT activation, hormonal changes—apply to all forms of cold exposure, but the magnitude of benefit from cold showers specifically remains less certain.
Research Gaps That Matter
Several important questions lack definitive answers:
- Optimal cold shower protocols: We don’t know the ideal water temperature, duration, or frequency specifically for blood sugar benefits.
- Long-term effects: Most studies track changes over weeks or months, not years. Will benefits continue, plateau, or require increasing intensity?
- Individual variation: Who responds best to cold therapy? Are there genetic or metabolic factors that predict success?
- Interaction with medications: How do cold showers affect diabetes medications, and are dose adjustments needed?
- Comparative effectiveness: How do blood sugar improvements from cold showers compare to other interventions like exercise or dietary changes?
The Bottom Line on Current Evidence
Cold exposure—including cold showers—shows genuine promise as a complementary approach for improving insulin sensitivity and glucose metabolism. The biological mechanisms are well-understood, and the broader cold therapy research is encouraging. However, cold showers should be viewed as a potential addition to, not a replacement for, proven diabetes management strategies.
The NIH emphasizes that comprehensive diabetes management requires multiple evidence-based approaches including diet, exercise, medication compliance, and regular monitoring. Cold therapy fits into this framework as an experimental adjunct therapy, not a standalone solution.
Frequently Asked Questions About Cold Showers and Blood Sugar
Yes, cold showers can help lower blood sugar through several mechanisms. When exposed to cold water, your body activates shivering thermogenesis, which causes your muscles to consume glucose for heat production. Additionally, cold exposure activates brown adipose tissue, which burns both glucose and fatty acids. Research indicates that repeated cold exposure improves insulin sensitivity and can reduce fasting glucose levels over time, though cold showers produce milder effects than ice baths. However, the blood sugar reduction is modest and should complement, not replace, standard diabetes management approaches.
Based on cold exposure research, consistency matters more than intensity. Studies showing metabolic benefits typically involved 3-5 cold exposure sessions per week. Start with 30 seconds of cold water at the end of your regular shower and gradually work up to 5-10 minutes over several weeks. Most participants in cold water immersion studies saw insulin sensitivity improvements after 4-8 weeks of regular practice. However, individual responses vary, and you should monitor your blood sugar levels closely to track your personal response. Always consult your healthcare provider before starting any cold therapy protocol.
Cold showers carry specific risks for people with diabetes and require medical guidance before starting. The cold shock response increases heart rate and blood pressure, which can be dangerous if you have cardiovascular complications from diabetes. Additionally, the CDC notes that cold exposure can affect blood circulation and potentially mask symptoms of hypoglycemia. If you have diabetic neuropathy, you might not properly sense temperature, increasing risk of cold injury. People with diabetes should only try cold showers with their doctor’s approval, starting very gradually and monitoring blood sugar before and after each session.
Ice baths involve full-body immersion in water at 40-50°F (4-10°C) for 10-20 minutes, creating intense cold exposure that strongly activates metabolic responses. Cold showers use warmer water (50-70°F) for 5-10 minutes and produce milder metabolic effects. Research shows that ice baths trigger more dramatic increases in brown fat activity, shivering thermogenesis, and glucose uptake compared to cold showers. However, ice baths also carry greater cardiovascular risks and are harder to maintain consistently. For blood sugar management, cold showers offer a safer, more accessible entry point with modest benefits, while ice baths may provide stronger metabolic effects but require more caution.
Yes, cold exposure can support both weight loss and blood sugar control through overlapping mechanisms. Cold temperatures activate brown adipose tissue, which burns calories to produce heat—potentially increasing daily energy expenditure by 100-300 calories with regular cold exposure. The shivering response also burns glucose and fatty acids. Studies show that cold acclimation improves metabolic rate and fat oxidation while enhancing insulin sensitivity. However, the weight loss effects are modest and work best when combined with proper diet and exercise. Think of cold exposure as a metabolic enhancer rather than a primary weight loss tool.
Yes, research demonstrates that repeated cold exposure improves insulin sensitivity in people with type 2 diabetes. A 2021 study showed that cold exposure reduced fasting glucose and insulin levels while improving insulin sensitivity markers. The mechanisms include increased adiponectin production (a hormone that protects against insulin resistance), enhanced glucose uptake by muscles during shivering, and improved brown fat activity. However, most research studied cold water immersion rather than cold showers specifically. The insulin sensitivity improvements are genuine but modest, typically showing 10-15% improvement in insulin sensitivity markers after 4-8 weeks of regular cold exposure.
Absolutely not. Cold showers should never replace prescribed diabetes medications or standard treatments. While cold exposure can improve insulin sensitivity and glucose metabolism, the effects are modest and don’t address all aspects of diabetes management. Diabetes medications are specifically calibrated to your individual needs and have extensive safety and efficacy data. Cold therapy is an experimental complementary approach that may enhance—but cannot substitute for—proven medical treatments. Always maintain your prescribed medication regimen, and discuss any complementary therapies, including cold showers, with your healthcare provider before starting.
Conclusion: Cold Showers as Part of Your Blood Sugar Strategy
The science behind cold showers and blood sugar control reveals a fascinating connection between temperature stress and metabolic health. When you expose your body to cold water, you trigger multiple physiological responses—shivering thermogenesis, brown adipose tissue activation, and hormonal changes—that can genuinely improve insulin sensitivity and glucose metabolism.
However, cold showers aren’t a magic solution for diabetes. The benefits are real but modest, and they come with safety considerations that matter more for people with diabetes or cardiovascular issues. Think of cold therapy as one tool in a comprehensive diabetes management toolkit, not a standalone solution or medication replacement.
If you’re considering cold showers for blood sugar control, the most important step is consulting your healthcare provider. They can assess your individual risk factors, help you start safely, and monitor how this practice affects your blood sugar patterns. Start gradually, monitor consistently, and be patient—metabolic adaptations take weeks to develop.
The research on cold exposure and diabetes continues to evolve. While we need more studies specifically on cold showers (versus ice baths or immersion), the underlying mechanisms are well-established. For some people, this accessible form of cold therapy may offer a safe way to enhance insulin sensitivity as part of a broader lifestyle approach to managing type 2 diabetes.
Remember: sustainable, consistent practices deliver better results than extreme measures. Whether you decide to try cold showers or not, the proven foundations of diabetes management—proper nutrition, regular physical activity, medication adherence, stress management, and quality sleep—remain your most powerful tools for blood sugar control.
References
- Ivanova YM, Mazurak N, Enck P. Examining the benefits of cold exposure as a therapeutic strategy for obesity and type 2 diabetes. PubMed. 2021. Available at: https://pubmed.ncbi.nlm.nih.gov/33764169/
- Espeland D, de Weerd L, Mercer JB. Health effects of voluntary exposure to cold water – a continuing subject of debate. PMC. 2022. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9518606/
- Case Western Reserve University. The science behind ice baths and polar plunges: Are they truly beneficial? Case.edu. 2025. Available at: https://case.edu/news/science-behind-ice-baths-and-polar-plunges-are-they-truly-beneficial
- Harvard Health Publishing. Cold plunges: Healthy or harmful for your heart? Harvard Health. 2025. Available at: https://www.health.harvard.edu/heart-health/cold-plunges-healthy-or-harmful-for-your-heart
- Centers for Disease Control and Prevention. Managing Diabetes in Cold Weather. CDC. 2024. Available at: https://www.cdc.gov/diabetes/articles/managing-diabetes-cold-weather.html
- National Institute of Diabetes and Digestive and Kidney Diseases. Low Blood Glucose (Hypoglycemia). NIDDK. 2024. Available at: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/low-blood-glucose-hypoglycemia
- National Institutes of Health. DASH-style diet helps control blood glucose. NIH Research Matters. 2025. Available at: https://www.nih.gov/news-events/nih-research-matters/dash-style-diet-helps-control-blood-glucose
- Nature Communications. Temperature regulation and glucose metabolism research. Nature. 2023. Available at: https://www.nature.com/articles/s41467-025-61499-2
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




