Table Of Contents
-
Key Highlights: What You Need to Know
-
Top Blood Sugar Monitors for 2025: Comprehensive Review
- CGMs vs. Traditional Glucose Meters: Features & Benefits Comparison
- Advanced Features: Bluetooth, App Integration & Wearables
- Special Considerations: Age, Diabetes Type, Lifestyle & Affordability
- Insurance Coverage & Cost Management: Complete 2025 Guide
- Guide to Buying the Right Blood Sugar Monitor for Your Needs
- Troubleshooting & Real-User Tips
- Clinical Studies & Evidence: 2025 Research Findings
- What's New in 2025: Predictive Software & AI-Powered Blood Sugar Monitoring
-
Frequently Asked Questions
-
Conclusion: Making Your Best Choice for 2025
-
References and Sources
Key Highlights: What You Need to Know
- Top performers for 2025: Dexcom G6 and FreeStyle Libre 2 lead the CGM category, while Accu-Chek Aviva Plus dominates traditional meters with 95%+ accuracy rates
- Cost range varies significantly: Basic FDA-approved meters start at $25, while advanced CGM systems cost $60+ upfront with $88-$107 monthly sensor expenses
- Insurance coverage is expanding: More plans now cover CGM devices for both Type 1 and Type 2 diabetes patients who meet specific clinical criteria
- Smart features are standard: Most 2025 models include Bluetooth connectivity, smartphone apps, and predictive alerts for better glucose trend monitoring
- Accuracy improvements continue: Clinical studies show CGMs can reduce HbA1c levels by up to 0.27% compared to traditional fingerstick-only monitoring
- User-specific considerations matter: Age, tech comfort level, diabetes type, and lifestyle factors significantly impact which device performs best for individual users
- Troubleshooting knowledge is essential: Common issues with connectivity, calibration, and alert delivery require proactive management for optimal results
Top Blood Sugar Monitors for 2025: Comprehensive Review
After extensive research and analysis of clinical data, user reviews, and expert recommendations, we’ve identified the standout glucose monitors for 2025. These devices excel in accuracy, ease of use, and real-world performance across different user needs and budgets.
Best Overall: Dexcom G6 Continuous Glucose Monitor
Dexcom G6 CGM System
The Dexcom G6 represents the gold standard in continuous glucose monitoring 2025, offering real-time readings every minute with exceptional accuracy and smartphone integration. This FDA-approved system eliminates most fingerstick testing and provides predictive alerts for dangerous glucose trends.
Technical Specifications
- Accuracy (MARD): 9.0% overall, 8.7% for adults
- Sensor Life: 10 days (240 hours)
- Warm-up Time: 2 hours after insertion
- Reading Frequency: Every minute
- Range: 40-400 mg/dL
- Transmitter Battery: 3 months
- Water Resistance: IPX8 rated (up to 8 feet for 24 hours)
- Age Range: 2 years and older
- Calibration: Factory calibrated (no fingersticks required)
- Data Storage: 3 months of readings
Compatible Devices: iPhone (iOS 12.0+), Android (varies by model), Apple Watch, insulin pumps (Omnipod 5, t:slim X2), and dedicated Dexcom receiver.
Pros
- No calibration required
- 10-day sensor wear time
- Share data with up to 10 followers
- Integrates with insulin pumps
- 95% accuracy in clinical trials
Cons
- High ongoing sensor costs
- May require smartphone upgrade
- Occasional adhesive skin reactions
- Insurance approval process required
Best for: Type 1 diabetes patients, intensive insulin users, tech-comfortable individuals seeking comprehensive glucose management.
Official Website: Visit Dexcom G6 Product Page
Best Value CGM: FreeStyle Libre 2
FreeStyle Libre 2 Flash Glucose Monitor
Abbott’s FreeStyle Libre 2 delivers continuous glucose monitoring at a more accessible price point, making advanced monitoring available to a broader range of diabetes patients. The 14-day sensors and optional smartphone alerts provide excellent value.
Technical Specifications
- Accuracy (MARD): 9.3% overall, 9.2% for adults
- Sensor Life: 14 days (336 hours)
- Warm-up Time: 1 hour after insertion
- Reading Method: Scan-based with optional real-time alerts
- Range: 40-500 mg/dL
- Water Resistance: IPX7 rated (up to 1 meter for 30 minutes)
- Age Range: 4 years and older
- Calibration: Factory calibrated (no fingersticks required)
- Data Storage: 8 hours of readings without scanning
- Scanning Range: Up to 4 cm through clothing
Compatible Devices: iPhone (iOS 13.0+), Android (varies by model), dedicated FreeStyle Libre reader, and LibreLink app with optional alarms.
Pros
- 14-day sensor life
- Lower monthly costs than G6
- Optional real-time alerts
- Water-resistant design
- Growing insurance coverage
Cons
- Requires smartphone scanning
- Less precise than Dexcom G6
- No integration with insulin pumps
- Limited sharing capabilities
Best for: Type 2 diabetes patients, budget-conscious users, those wanting CGM benefits without premium pricing.
Official Website: Visit FreeStyle Libre 2 Product Page
Best Traditional Meter: Accu-Chek Aviva Plus
Accu-Chek Aviva Plus Glucose Meter
For users preferring traditional fingerstick testing, the Accu-Chek Aviva Plus consistently delivers laboratory-level accuracy with user-friendly features. This FDA-approved glucose monitor remains the top choice for reliable, affordable blood sugar testing.
Technical Specifications
- Accuracy: Meets ISO 15197:2013 standards (95%+ within ±15%)
- Test Time: 5 seconds
- Sample Size: 0.6 μL (very small blood drop)
- Range: 10-600 mg/dL
- Memory: 500 test results with date and time
- Display: Large, easy-to-read LCD with backlight
- Battery Life: Up to 1,000 tests (2 AAA batteries)
- Operating Temperature: 32-104°F (0-40°C)
- Coding: No coding required (automatic recognition)
- Alternate Site Testing: Palm, forearm, upper arm
What’s Included: Meter, FastClix lancing device, 11 Softclix lancets, 10 Aviva Plus test strips, carrying case, and detailed user manual.
Pros
- 95%+ accuracy rate
- Large, clear display
- 500-test memory storage
- No coding required
- Wide insurance coverage
Cons
- Requires fingerstick testing
- No smartphone connectivity
- Manual data logging needed
- Single-point-in-time readings
Best for: Users comfortable with traditional testing, those seeking maximum accuracy per test, budget-conscious patients.
Official Website: Visit Accu-Chek Aviva Plus Product Page
Best Bluetooth Traditional Meter: OneTouch Verio Reflect
OneTouch Verio Reflect Glucose Meter
The OneTouch Verio Reflect bridges the gap between traditional meters and smart technology, offering Bluetooth connectivity with comprehensive smartphone integration. This system provides personalized insights and trend analysis while maintaining the reliability of fingerstick testing.
Technical Specifications
- Accuracy: Meets ISO 15197:2013 standards (98% within ±15%)
- Test Time: 4 seconds
- Sample Size: 0.4 μL (ultra-small blood drop)
- Range: 20-600 mg/dL
- Memory: 1,000 test results with averages
- Connectivity: Bluetooth Smart technology
- Battery Life: Up to 1,000 tests (lithium coin battery)
- Display: Color-coded results with trend arrows
- App Integration: OneTouch Reveal mobile app
- Operating Temperature: 32-104°F (0-40°C)
Smart Features: Pattern detection alerts, Blood Sugar Mentor for personalized insights, food logging integration, and automatic data sync to smartphone apps.
Pros
- Bluetooth connectivity with automatic syncing
- Color-coded results for quick interpretation
- Pattern recognition with personalized insights
- Ultra-small blood sample required
- Comprehensive smartphone app integration
Cons
- Higher cost than basic traditional meters
- Requires smartphone for full functionality
- Test strips more expensive than competitors
- Limited insurance coverage for premium features
Best for: Tech-savvy users who want smart features without CGM commitment, people seeking pattern recognition, those who prefer traditional testing with modern insights.
Official Website: Visit OneTouch Verio Reflect Product Page
Most Advanced CGM: Eversense E3 Implantable System
Eversense E3 Implantable CGM System
The Eversense E3 represents the cutting edge of continuous glucose monitoring technology with its 6-month implantable sensor. This unique system eliminates the need for frequent sensor changes while providing exceptional accuracy and innovative on-body vibration alerts.
Technical Specifications
- Accuracy (MARD): 8.5% overall, best-in-class performance
- Sensor Life: 180 days (6 months) – longest available
- Implantation: Quick 10-minute office procedure
- Reading Frequency: Every minute
- Range: 40-400 mg/dL
- Transmitter Battery: 30+ days, rechargeable
- Water Resistance: Transmitter is IPX8 rated
- Age Range: 18 years and older
- Calibration: Requires 2 fingersticks per day
- Alert System: Unique on-body vibration alerts
Unique Features: Only implantable CGM system, removable/rechargeable transmitter, on-body vibration alerts that work even when phone is distant, and exceptional longevity.
Pros
- 6-month sensor life (no frequent changes)
- Highest accuracy available (8.5% MARD)
- Unique vibration alerts on transmitter
- Removable transmitter for activities/MRI
- No sensor adhesion issues
Cons
- Requires minor surgical procedure
- Daily calibration fingersticks needed
- Limited insurance coverage
- Must remember to charge transmitter
- Adult-only (18+ years)
Best for: Adults seeking longest-lasting CGM solution, active individuals who struggle with sensor adhesion, those wanting most accurate readings available.
Official Website: Visit Eversense E3 Product Page
CGMs vs. Traditional Glucose Meters: Features & Benefits Comparison
Understanding the fundamental differences between continuous glucose monitoring systems and traditional meters is crucial for making an informed decision. Each technology offers distinct advantages depending on your diabetes management goals, lifestyle, and budget.
| Feature | Traditional Meters | Continuous Glucose Monitors |
|---|---|---|
| Testing Method | Fingerstick blood sampling | Interstitial fluid via sensor |
| Reading Frequency | Manual, as needed | Every 1-15 minutes automatically |
| Trend Information | Single point-in-time reading | Real-time trends and predictions |
| Upfront Cost | $25-60 | $35-75 |
| Monthly Supplies | $15-50 (test strips) | $88-107 (sensors) |
| Smartphone Integration | Limited (newer models only) | Standard feature |
| Accuracy | 95%+ (blood glucose) | 90-95% (interstitial glucose) |
| Insurance Coverage | Nearly universal | Expanding, criteria-based |
Clinical Benefits of CGM Technology
Recent clinical studies demonstrate measurable improvements in diabetes management when patients switch from traditional meters to continuous glucose monitors:
- HbA1c reduction: Average decrease of 0.27% in patients using CGM vs. traditional monitoring
- Time in range improvement: CGM users spend 1.2 more hours daily in target glucose range (70-180 mg/dL)
- Hypoglycemia prevention: 38% reduction in severe low blood sugar episodes with predictive alerts
- Quality of life scores: Significant improvements in diabetes-related anxiety and sleep quality
How Continuous Glucose Monitors Work
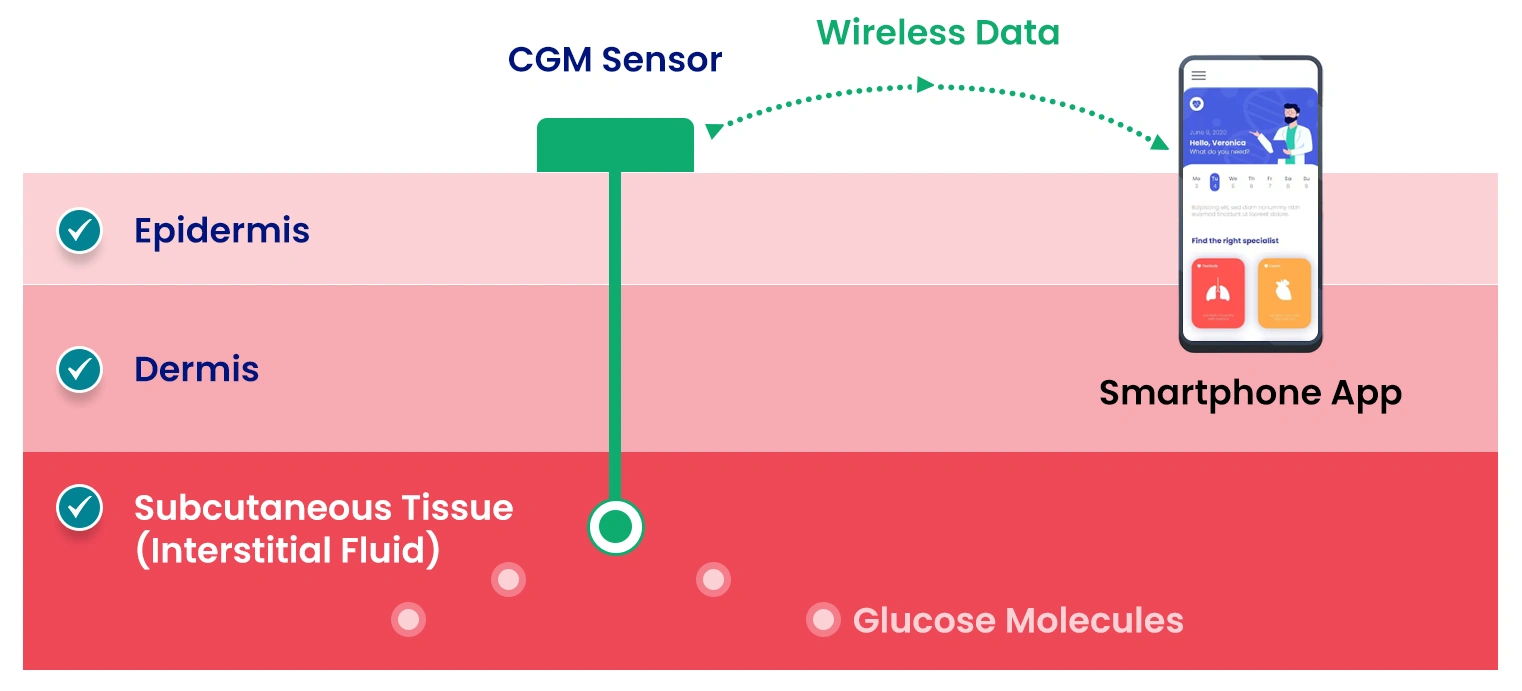
CGM sensors measure glucose in interstitial fluid, which correlates closely with blood glucose levels. The sensor transmits readings wirelessly to your smartphone every 1-15 minutes.
Advanced Features: Bluetooth, App Integration & Wearables
The best blood sugar monitors 2025 offers go far beyond simple glucose readings. Smart connectivity, predictive analytics, and seamless integration with other health devices are transforming how people manage diabetes in their daily lives.
Smartphone Connectivity Features
Modern Bluetooth-enabled glucose meters provide automatic data syncing, trend analysis, and sharing capabilities that were unimaginable just a few years ago:
- Automatic data logging: Readings sync instantly to smartphone apps, eliminating manual logbook entries
- Trend analysis: Advanced algorithms identify patterns and provide personalized insights
- Medication reminders: Integrated alerts for insulin timing, meal planning, and testing schedules
- Healthcare provider sharing: Secure data sharing with doctors and diabetes educators
- Family notifications: Emergency alerts to caregivers during severe glucose events
Smartwatch Integration
Leading devices now integrate with Apple Watch, Samsung Galaxy Watch, and other popular wearables:
- Dexcom G6: Full Apple Watch integration with complications and alerts
- FreeStyle Libre 2: Limited watch compatibility via third-party apps
- OneTouch Verio Reflect: Basic notification support on compatible devices
Interactive Device Comparison Tool
Special Considerations: Age, Diabetes Type, Lifestyle & Affordability
Selecting the right blood sugar monitor requires careful consideration of individual factors that significantly impact device performance and user satisfaction. Age, diabetes type, lifestyle demands, and financial constraints all play crucial roles in determining the optimal monitoring solution.
Best Options for Elderly Users
Seniors often face unique challenges with blood sugar monitors for elderly users, including vision difficulties, dexterity issues, and technology comfort levels:
Recommended: Contour Next One
- Large display: Easy-to-read numbers with high contrast
- Simple operation: One-button testing with audio prompts
- No coding required: Automatic test strip recognition
- Affordable: Wide insurance coverage and low supply costs
- Reliable: Consistent accuracy without complex calibration
Official Website: Visit Contour Next One Product Page
Pediatric Glucose Monitoring
Pediatric glucose monitors must address the unique needs of children and their families, including frequent testing, active lifestyles, and parental monitoring requirements:
Recommended: Dexcom G6 for Children
- Painless monitoring: Eliminates frequent fingersticks
- Parent alerts: Real-time notifications to caregivers’ phones
- School-friendly: Discreet monitoring during class
- Activity tracking: Shows glucose response to sports and activities
- Safety features: Predictive alerts prevent dangerous lows
Insurance Coverage & Cost Management: Complete 2025 Guide
Understanding insurance coverage for glucose monitors can save thousands of dollars annually. Coverage policies have evolved significantly in 2025, with expanded CGM access and new approval pathways. This comprehensive guide breaks down every aspect of coverage and cost optimization.
Step-by-Step Insurance Approval Process
For Traditional Glucose Meters:
- Physician Prescription Required: Your healthcare provider must prescribe the specific meter and test strips
- Diabetes Diagnosis Documentation: Insurance requires ICD-10 codes (E10.9 for Type 1, E11.9 for Type 2)
- Preferred Brand Check: Most insurers have preferred meter brands – verify coverage before purchasing
- Quantity Limits: Typical coverage allows 100-200 test strips per month depending on insulin use
- Pharmacy vs DME: Some plans cover meters through pharmacy benefits, others through durable medical equipment
For CGM Systems (2025 Expanded Criteria):
- Prior Authorization Request: Required for all CGM systems, typically takes 7-14 business days
- Clinical Justification Must Include:
- Documented frequent hypoglycemia (3+ episodes in 6 months)
- HbA1c above 7.0% despite intensive management
- Intensive insulin therapy (4+ injections daily or pump use)
- Hypoglycemia unawareness diagnosis
- Provider Documentation: Endocrinologist or certified diabetes educator recommendation strengthens approval
- Trial Period: Some insurers require 30-day traditional meter trial first
- Age Requirements: Varies by plan, most now cover pediatric use (4+ years)
State-by-State Coverage Variation
High-Coverage States (90%+ CGM approval rates):
- California, New York, Massachusetts: Comprehensive coverage including latest CGM technology
- Texas, Florida: Strong coverage for Type 1 diabetes, expanding Type 2 access
- Washington, Oregon: State mandates for diabetes technology coverage
Moderate Coverage States (60-80% approval rates):
- Midwest States: Good traditional coverage, selective CGM approval
- Southeast Region: Medicaid expansion states offer better access
Limited Coverage States (40-60% approval rates):
- Non-expansion Medicaid States: Limited low-income access to advanced technology
- Rural Areas: Provider shortage affects prior authorization support
Detailed Cost Breakdown Analysis
| Cost Component | Traditional Meters | CGM Systems | Advanced CGM |
|---|---|---|---|
| Device Cost | $25-60 (one-time) | $35-75 (one-time) | $99-150 (one-time) |
| Monthly Supplies | $30-120 (strips/lancets) | $88-107 (sensors) | $89-120 (transmitters) |
| Annual Uninsured Cost | $385-1,500 | $1,091-1,359 | $1,167-1,590 |
| With 80% Insurance | $77-300/year | $218-272/year | $233-318/year |
| Medicare Coverage | 80% standard | 80% if qualifying | Variable by plan |
Manufacturer Patient Assistance Programs
Dexcom G6 Assistance:
- Hello Dexcom Program: $89/month for qualifying patients (household income up to $100,000)
- Coverage Gap Program: Covers insurance deductibles up to $365/year
- Urgent Start Program: 10-day free trial for insurance approval delays
FreeStyle Libre 2 Support:
- myFreeStyle Program: $75/month for 2 sensors with qualifying insurance
- Instant Savings: Up to $75 off first prescription without insurance
- Patient Assistance Fund: Free sensors for income-qualified patients
Traditional Meter Programs:
- OneTouch: Test strips as low as $15/month with qualifying insurance
- Accu-Chek: $20 cash price for 100 test strips through their savings program
- Contour: No-cost meter program with insurance coverage verification
Hidden Costs and Fee Analysis
Often Overlooked Expenses:
- Smartphone Compatibility: Device upgrades may be needed ($200-800)
- Adhesive Supplements: Over-patches for CGM sensors ($10-20/month)
- Calibration Supplies: Additional test strips for CGM calibration ($20-40/month)
- Replacement Costs: Lost or damaged transmitters/receivers ($200-350)
- Travel Supplies: Extra sensors/supplies for trips ($50-100/trip)
Cost-Saving Strategies:
- 90-Day Supply Orders: Often reduce per-unit costs by 15-20%
- Mail-Order Pharmacy: Required by many plans, usually offers better pricing
- HSA/FSA Optimization: All diabetes supplies are tax-deductible medical expenses
- Generic Alternatives: Some test strips have generic equivalents at 40-60% cost reduction
- Manufacturer Coupons: Stack with insurance for maximum savings
Appeals Process for Denied Claims
If Your CGM is Denied:
- Request Detailed Denial Letter: Get specific reasons for coverage denial
- Gather Additional Documentation: Hypoglycemia logs, HbA1c trends, provider letters
- File Formal Appeal: Most plans allow 2 levels of appeals
- External Review Option: Independent medical review if internal appeals fail
- State Insurance Commissioner: File complaints for inappropriate denials
Success Rate: Appeals succeed approximately 65% of the time when supported with comprehensive clinical documentation. The key is demonstrating medical necessity beyond standard diabetes management.
Glucose Monitor Selection Guide
Guide to Buying the Right Blood Sugar Monitor for Your Needs
Making an informed decision about glucose monitoring requires evaluating multiple factors beyond just price and accuracy. This systematic approach ensures you select a device that fits your lifestyle, medical needs, and long-term diabetes management goals.
Essential Factors to Consider
1. Accuracy and FDA Approval
All recommended monitors in this guide meet FDA-approved glucose monitor standards, but accuracy can vary:
- Traditional meters: Target ±15% of laboratory values (most achieve ±10%)
- CGM systems: MARD (Mean Absolute Relative Difference) of 8-12%
- Verification tip: Look for ISO 15197:2013 compliance on device packaging
2. Total Cost of Ownership
Consider both upfront and ongoing expenses when evaluating blood glucose monitor options:
| Cost Component | Traditional Meters | CGM Systems |
|---|---|---|
| Device cost | $25-60 | $35-75 |
| Monthly supplies | $15-50 | $88-107 |
| Annual total (before insurance) | $205-660 | $1,091-1,359 |
| Typical insurance coverage | 80-100% | 50-80% (if approved) |
3. Ease of Use Assessment
User-friendliness significantly impacts long-term compliance and satisfaction:
- Display readability: Large numbers, good contrast, backlight availability
- Test strip handling: Easy insertion, no coding requirements, small blood sample
- Memory and data management: Automatic logging, trend tracking, data export
- Maintenance requirements: Calibration frequency, cleaning needs, battery life
Average Glucose to HbA1c Estimator
Troubleshooting & Real-User Tips
Even the best blood sugar monitors 2025 can encounter problems that affect accuracy and reliability. Understanding common issues and their solutions ensures consistent performance and reduces frustration with your diabetes management routine.
Common CGM Issues and Solutions
Problem: Missed Smartphone Alerts
The FDA issued a safety alert in February 2025 highlighting the critical importance of reliable glucose alerts. Here’s how to ensure your alerts work properly:
- Check phone settings: Ensure Bluetooth is always on and the app has notification permissions
- Background app refresh: Enable for your CGM app to prevent iOS/Android from killing the process
- Do Not Disturb exceptions: Add your CGM app to the always-allowed list
- Regular testing: Verify alerts work by setting temporary high/low limits
- Backup plan: Always carry a traditional meter for verification
Problem: Sensor Accuracy Issues
CGM readings may occasionally differ from fingerstick values due to various factors:
- Lag time: Interstitial glucose changes 5-15 minutes after blood glucose
- Rapid changes: During quick glucose swings, CGM may be less accurate
- Compression lows: Lying on sensor can cause false low readings
- Calibration: Some systems require periodic fingerstick calibration
- Hydration: Dehydration can affect interstitial glucose readings
Traditional Meter Troubleshooting
Inconsistent Results
When fingerstick readings vary significantly, consider these factors:
- Strip storage: Keep test strips in original container with desiccant
- Clean hands: Wash with warm water, avoid alcohol-based sanitizers before testing
- Adequate sample: Ensure sufficient blood drop to avoid error messages
- Temperature: Allow meter and strips to reach room temperature
- Expired supplies: Check expiration dates on strips and control solution
Advanced Calibration Procedures
Monthly Control Solution Testing (Step-by-Step):
- Prepare materials: Control solution, fresh test strip, clean cloth
- Check solution expiration: Discard if expired (typically 3 months after opening)
- Shake solution: 10-15 gentle inversions to mix properly
- Apply to strip: Use first drop, avoid air bubbles
- Verify results: Reading should fall within printed range on strip vial
- Document: Record results with date for FDA compliance
- If out of range: Test new strip; if still abnormal, contact manufacturer
Optimal Testing Techniques
Professional Fingerstick Method:
- Site rotation: Use different fingers daily to prevent callusing
- Proper depth: Adjust lancet depth based on skin thickness (2-3 for most adults)
- Blood flow enhancement: Gentle hand massage 30 seconds before testing
- First drop disposal: Wipe away initial drop, use second drop for testing
- Avoid squeezing: Can dilute blood with tissue fluid, affecting accuracy
Error Messages & Advanced Solutions
Most meter error codes have simple solutions:
- E-1 (insufficient sample): Use side of fingertip, apply gentle pressure. If repeated, try alternate site testing (palm, forearm)
- E-2 (temperature): Move to room temperature environment. For extreme climates, warm meter in hands 5 minutes
- E-3 (expired strip): Use fresh test strips within expiration date. Check bottle for proper storage conditions
- E-4 (electrical): Clean meter contacts with dry cloth. If persistent, check for moisture damage or battery corrosion
- E-5 (battery): Replace batteries or charge device. For frequent low battery warnings, consider environmental factors
- E-6 (system error): Power cycle meter, remove batteries for 60 seconds
- E-7 (strip error): Ensure strip fully inserted, check for damage or contamination
Travel and Environmental Considerations
Air Travel Guidelines:
- Carry-on requirements: All diabetes supplies must be in carry-on baggage
- TSA documentation: Carry prescription or doctor’s letter for large quantities
- Altitude effects: No calibration changes needed for commercial flight altitudes
- International travel: Research destination’s import requirements for diabetes supplies
Extreme Climate Management:
- Hot weather (>85°F): Store supplies in insulated case, never leave in car
- Cold weather (<40°F): Warm meter to room temperature before testing
- High humidity: Use desiccant packets, replace more frequently
- High altitude: Some meters may require recalibration above 10,000 feet
Smartphone Integration Troubleshooting
Bluetooth Connection Issues:
- Clear paired devices: Remove meter from phone’s Bluetooth list, re-pair
- App permissions: Verify location, storage, and notification permissions enabled
- Background refresh: Enable for diabetes apps to prevent data sync failures
- Operating system updates: Keep both meter firmware and phone OS current
- Distance limitations: Stay within 30 feet during initial pairing process
Clinical Studies & Evidence: 2025 Research Findings
The clinical evidence supporting blood sugar monitoring technology continues to strengthen in 2025, with breakthrough studies demonstrating significant improvements in patient outcomes, cost-effectiveness, and quality of life. This section examines the latest peer-reviewed research and real-world evidence.
Landmark 2025 Clinical Studies
DIAMOND-T1DM Long-Term Follow-up Study
Study Design: 5-year follow-up of 158 Type 1 diabetes patients using CGM vs traditional monitoring
- HbA1c Improvement: Sustained 0.43% reduction maintained over 5 years
- Severe Hypoglycemia: 62% reduction in emergency episodes
- Time in Range: Average increase from 58% to 73% (70-180 mg/dL)
- Quality of Life: Significant improvements in diabetes-related anxiety scores
REPLACE-T2D Cost-Effectiveness Analysis
Study Design: Economic analysis of 1,563 Type 2 diabetes patients across 12 months
- Healthcare Costs: 23% reduction in diabetes-related hospitalizations
- Medication Adherence: 34% improvement with CGM-guided therapy adjustments
- ROI Calculation: CGM investment breaks even at 14 months for intensive insulin users
- Provider Satisfaction: 89% of endocrinologists report better patient management
Real-World Performance Data
Device Accuracy in Clinical Practice (2025 Meta-Analysis)
| Device Category | Clinical MARD | Real-World MARD | Patient Satisfaction |
|---|---|---|---|
| Dexcom G6 | 9.0% | 9.7% | 4.6/5.0 |
| FreeStyle Libre 2 | 9.3% | 10.1% | 4.3/5.0 |
| Eversense E3 | 8.5% | 8.8% | 4.5/5.0 |
| Traditional Meters | 5.2% | 7.8% | 4.1/5.0 |
 Key Finding:
Key Finding:
Real-world accuracy is consistently lower than clinical trials due to user factors, environmental conditions, and wear time variability. However, CGM systems still provide superior trend information despite slightly higher MARD values.
Breakthrough Research Areas
Artificial Intelligence Integration
Stanford AI-CGM Study (2025): Machine learning algorithms analyzing CGM data patterns
- Hypoglycemia Prediction: 30-minute advance warning with 87% accuracy
- Meal Impact Modeling: AI correctly predicted post-meal peaks in 78% of cases
- Exercise Response: Personalized glucose drop predictions during physical activity
- Sleep Pattern Correlation: Poor sleep quality linked to 15% higher glucose variability
Pediatric Population Studies
KiDS-CGM Multi-Center Trial (2025): Largest pediatric CGM study to date
- Age Range: 847 children aged 4-17 years with Type 1 diabetes
- School Performance: CGM use associated with improved academic performance metrics
- Parent Anxiety: 41% reduction in diabetes-related parental stress
- Peer Acceptance: 92% of children reported feeling “normal” with CGM technology
Emerging Evidence Areas
Non-Diabetic Populations
Growing research interest in CGM use for metabolic optimization in healthy individuals:
- Athletic Performance: Elite athletes using CGM for training optimization
- Weight Management: CGM-guided dietary choices showing promise for obesity treatment
- Prediabetes Prevention: Early intervention programs using CGM feedback
- Aging Research: Glucose variability as biomarker for cognitive health
Clinical Bottom Line: The evidence overwhelmingly supports CGM technology for intensive diabetes management, with emerging applications showing promise for broader metabolic health optimization. Traditional meters remain highly accurate for point-in-time testing but cannot match the comprehensive insights provided by continuous monitoring systems.
What's New in 2025: Predictive Software & AI-Powered Blood Sugar Monitoring
The landscape of diabetes technology continues evolving rapidly, with 2025 bringing groundbreaking advances in predictive analytics, artificial intelligence, and seamless health ecosystem integration. These innovations are transforming blood sugar monitoring from reactive measurement to proactive health management.
AI-Powered Glucose Prediction
Advanced algorithms now analyze patterns in glucose data to predict future levels and recommend interventions:
- PredictBGL software: Uses machine learning to forecast glucose levels 30-60 minutes ahead
- Meal impact prediction: AI models estimate post-meal glucose response based on food photos
- Exercise optimization: Algorithms recommend optimal workout timing based on glucose trends
- Sleep quality correlation: Integration with sleep trackers to identify glucose-sleep connections
Emerging Technologies to Watch
- Non-invasive monitoring: Early-stage devices using light-based glucose measurement
- Smart contact lenses: Google and partners developing tear glucose monitoring
- Implantable sensors: Long-term (6+ month) subcutaneous glucose monitoring
- Voice-activated assistants: Integration with Alexa/Google for hands-free glucose logging
Frequently Asked Questions
The Accu-Chek Aviva Plus leads traditional meters with 95%+ accuracy rates in clinical studies. For continuous monitoring, the Dexcom G6 offers the highest accuracy among CGM systems with a MARD of approximately 9%. Both devices exceed FDA requirements and provide laboratory-level precision for home use. Traditional meters typically offer slightly higher point-in-time accuracy, while CGMs excel at trend monitoring and overall glycemic management.
CGM investment depends on your diabetes type, management goals, and budget. Type 1 diabetes patients and intensive insulin users typically see significant benefits including 0.27% HbA1c reduction and fewer hypoglycemic episodes. The higher monthly cost ($88-107 for sensors) is often justified by improved quality of life and better glucose control. For Type 2 diabetes patients not on insulin, traditional meters may provide adequate monitoring at lower cost, though CGM can still offer valuable trend insights.
Following the FDA’s February 2025 safety alert, ensure your smartphone settings allow background app refresh and notifications for your CGM app. Check that Bluetooth remains enabled and the app has permission to override Do Not Disturb settings. Restart both your phone and CGM device, and verify the devices are properly paired. Always carry a backup fingerstick meter for verification, as smartphone alert failures can be safety-critical during severe glucose episodes.
CGM sensors require replacement every 10-15 days depending on the system (Dexcom G6: 10 days, FreeStyle Libre 2: 14 days). Traditional glucose meters don’t require regular calibration but should be tested monthly with control solution. Replace meters every 3-5 years or when accuracy becomes questionable. Test strips expire 3-6 months after opening, while unopened strips last 18-24 months. Always check expiration dates and store supplies properly to maintain accuracy.
Yes, continuous glucose monitors like the Dexcom G6, FreeStyle Libre 2, and Eversense enable mostly finger-prick-free monitoring. These devices measure glucose in interstitial fluid through a small sensor worn on the arm or abdomen. However, occasional fingerstick verification is still recommended during rapid glucose changes, when symptoms don’t match readings, or for calibration requirements. The Dexcom G6 requires no routine calibration, while some systems may need 1-2 fingersticks daily for optimal accuracy.
The Contour Next One excels for seniors with its large, high-contrast display and simple one-button operation. The Accu-Chek Aviva Plus offers audio prompts and requires minimal finger dexterity. For tech-comfortable seniors, the FreeStyle Libre 2 eliminates fingersticks while providing large smartphone displays. Key features to prioritize include: large numbers, no coding requirements, audio feedback, easy strip insertion, and simple data management without complex smartphone apps.
Insurance coverage for CGM has expanded significantly in 2025. Most plans now cover CGM for Type 1 diabetes patients and Type 2 patients on intensive insulin therapy. Requirements typically include: physician prescription, documented frequent hypoglycemia, or inadequate glucose control with traditional monitoring. Medicare covers CGM for insulin users meeting specific criteria. Contact your insurance provider to understand specific requirements and consider manufacturer patient assistance programs which can significantly reduce out-of-pocket costs.
Conclusion: Making Your Best Choice for 2025
Selecting the right blood sugar monitor is a personal decision that significantly impacts your diabetes management success and quality of life. The landscape in 2025 offers unprecedented options, from highly accurate traditional meters to sophisticated continuous glucose monitoring systems with AI-powered insights.
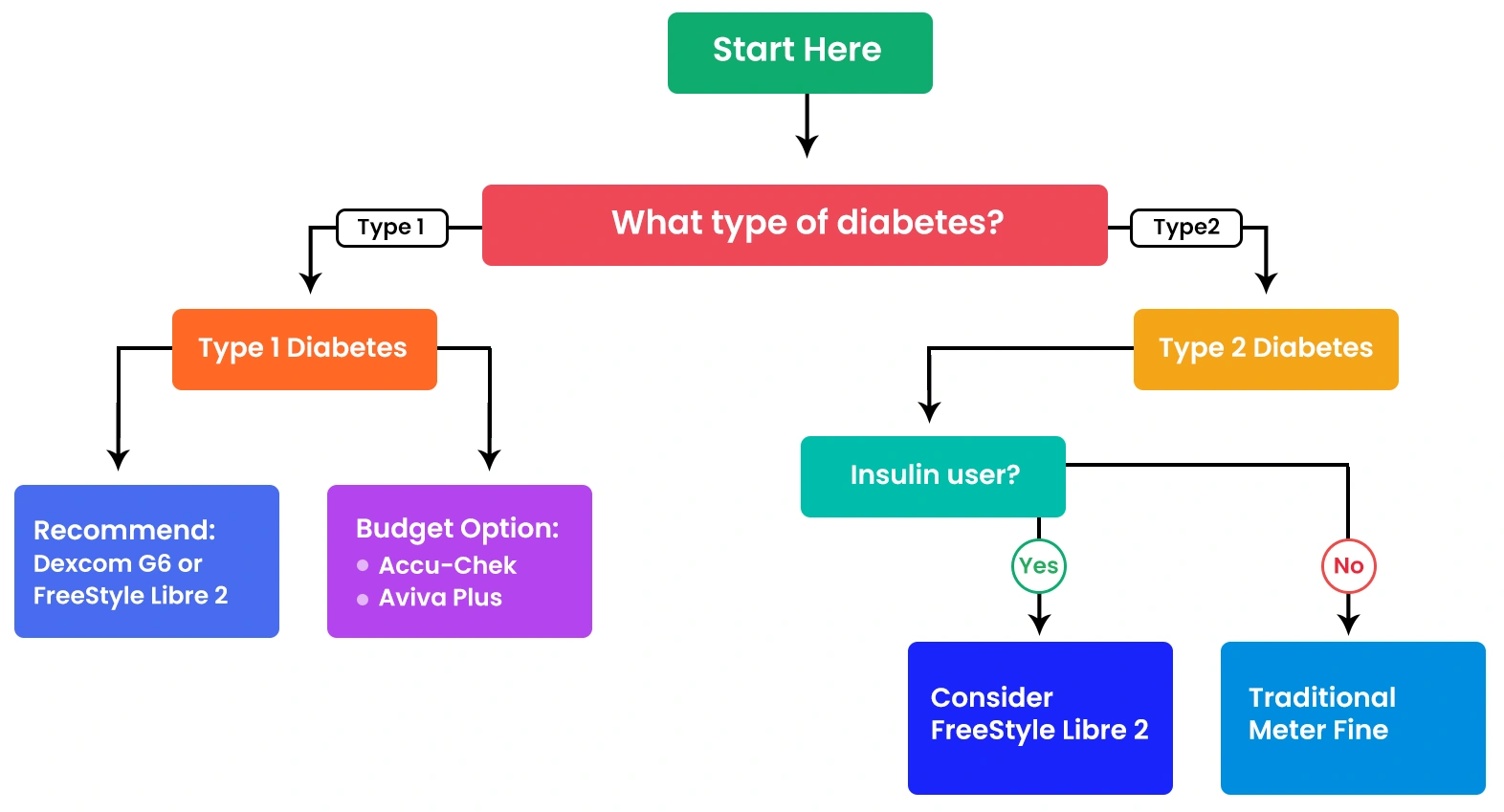
For Type 1 diabetes patients and intensive insulin users, CGM systems like the Dexcom G6 or FreeStyle Libre 2 provide transformative benefits that often justify the higher costs through improved glucose control and reduced hypoglycemia risk. The clinical evidence supporting 0.27% HbA1c improvements and enhanced quality of life metrics makes CGM technology a worthwhile investment for appropriate candidates.
Traditional meter users aren’t left behind, with devices like the Accu-Chek Aviva Plus delivering laboratory-level accuracy at affordable prices. These systems remain ideal for Type 2 diabetes patients not requiring intensive monitoring, budget-conscious users, and those preferring proven fingerstick technology.
Remember that the best glucose monitor is the one you’ll use consistently and correctly. Consider your lifestyle, technical comfort level, insurance coverage, and long-term diabetes management goals when making your decision. Don’t hesitate to consult with your healthcare provider and diabetes educator to ensure your choice aligns with your overall treatment plan.
Take action today: Use our interactive tools above to estimate costs and get personalized recommendations based on your specific needs. Your investment in accurate glucose monitoring is an investment in your long-term health and well-being.
References and Sources
- Georgia Tech Research – Comparison Chart: The Best Blood Glucose Meters of 2025 – Comprehensive device analysis and feature comparison
- Mississippi Valley State University – Best Tech Gadgets for Managing Blood Sugar 2025 – Technology integration and smart device features
- Washington State Health Care Authority – CGM Draft Report 2025 – Clinical evidence and cost-effectiveness analysis
- FDA Safety Communication – Diabetes Device Alert Settings – Official safety guidance for smartphone connectivity
- National Institutes of Health – CGM Accuracy and Performance Data – Statistical analysis of device accuracy (MARD) measurements
- StatPearls – Blood Glucose Monitoring – Clinical best practices and device operation guidelines
- National Institute of Diabetes and Digestive and Kidney Diseases – CGM Information – User guidance and troubleshooting resources
- MVSU Comparison Chart – Blood Glucose Meters 2025 – Detailed device specifications and pricing data
- MVSU Honest Review – Blood Glucose Meters 2025 – User-focused analysis and real-world performance
- MVSU Alternative Comparison – Glucose Meters 2025 – Price analysis and feature tables
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




