Table Of Contents
-
Key Highlights
- Exploring Peptides: From Biology To Weight-Loss Therapy
-
Determining Eligibility For Peptide-Based Weight Loss Therapy
-
Why Therapeutic Peptides Are Gaining Traction In Modern Weight Management
-
The Best Peptides For Weight Loss: A Research-Based Breakdown
-
Combination Therapies & Other Experimental Peptides
-
Risks, Challenges & Optimization Strategies
-
Lifestyle Tweaks That Supercharge Peptide Results
-
Frequently Asked Questions (FAQs)
-
Making Smart Weight-Loss Decisions With MD Pilot
-
References:
Despite numerous diets and exercise plans, 80-85% of people who lose significant weight eventually regain it. The underlying reason isn’t a lack of discipline—it’s biology. Our bodies are hardwired to resist long-term weight loss by slowing metabolism and increasing hunger to restore balance.
That’s where peptides are receiving growing attention in metabolic and obesity medicine. They work by influencing natural body signals that control hunger, energy use, and fat storage. This helps you lose weight and keep it off longer. However, with multiple choices and conflicting claims, finding the best peptides for weight loss can be confusing.
This guide will simplify it for you. We will explain how peptides promote weight loss, discuss the top options, outline the associated risks, and provide insights on selecting the best option for your body. By the end, you will also learn the questions to ask your healthcare provider, so you can make safe and informed decisions that lead to lasting results.
Key Highlights
- Peptides are emerging as powerful tools for sustainable weight loss by working with your body’s natural hormones and metabolic systems.
- Unlike crash diets, peptide therapies help regulate appetite, improve metabolism, and make it easier to maintain results in the long term.
- FDA-approved options, such as Semaglutide (Wegovy), Liraglutide (Saxenda), and Tirzepatide (Zepbound), are among the best peptides for weight loss, having demonstrated significant fat reduction and proven safety.
- Combining peptide therapy with a balanced diet, regular exercise, and medical supervision can enhance effectiveness and minimize side effects.
- Understanding peptide types, risks, and lifestyle integration enables you to make informed, safe, and personalized decisions for weight loss.
Exploring Peptides: From Biology To Weight-Loss Therapy
To understand how the best peptides for weight loss work, it is helpful first to explore what they are and their function. By grasping these basics, you will see why peptides are emerging as a powerful instrument in modern weight management.
Understanding Peptides & Their Influence
Peptides are short chains of amino acids, smaller than whole proteins, that serve as key messengers in the body. They help regulate numerous biological processes, including metabolism, hormone secretion, immune response, and tissue repair.
Your body naturally produces hundreds of these short chains of amino acids daily. For example, insulin is a peptide that regulates glucose absorption, while glucagon-like peptide-1 (GLP-1) helps control blood sugar levels by stimulating the release of insulin. These natural peptides show how precise signaling can influence metabolism and energy balance.
What Is Peptide Therapy?
Peptide therapy harnesses the biological power of peptides to improve health and influence specific bodily processes. This therapy can involve either naturally occurring or synthetic peptides designed to mimic or enhance the effects. For instance, some athletes use growth hormone-releasing peptides to support muscle recovery and bone health after training or competition.
Today, more than 100 peptide drugs are FDA-approved in the U.S., reflecting their growing role in treating metabolic, endocrine, and obesity-related conditions. A comprehensive research published on MDPI highlights the ever-increasing role of peptide therapeutics in obesity management. This emphasizes their potential to support metabolic health safely and effectively.
To understand how peptide therapy supports weight loss specifically, it helps to look at the body’s gut hormone and peptide systems. These systems play a central role in regulating appetite, metabolism, and overall energy balance.
The Role Of Gut Hormones & Peptide Systems
Gut hormones are naturally produced by the stomach, small intestine, and pancreas to regulate digestion, nutrient absorption, and gut movement. Beyond these functions, they play a crucial role in influencing energy balance and appetite by signaling brain regions that regulate hunger and satiety.
Many naturally occurring weight-loss peptides, such as GLP-1 (glucagon-like peptide-1) and PYY (peptide YY or peptide tyrosine tyrosine), are designed to work in conjunction with these systems. For example, PYY is released after meals and signals the brain to reduce hunger. In obesity medicine, therapeutic peptides utilize these mechanisms to restore healthier hormone responses, facilitating weight loss—rather than relying solely on strict caloric restriction.
Determining Eligibility For Peptide-Based Weight Loss Therapy
By clearly understanding eligibility, patients and clinicians can make informed decisions, ensuring that peptide therapy is used where it is most likely to be safe, effective, and sustainable. To be eligible for peptide-based weight-loss treatments, you would need to meet the following criteria:
- Have a BMI of 30 or higher
- Or, have a BMI of 27 or higher with a weight-related condition, such as high blood pressure, type 2 diabetes, or high cholesterol
- Struggle to achieve sustainable results through lifestyle changes alone, including diet and exercise
- Should not have contraindications, such as a history of thyroid cancer or an increased risk of pancreatitis
- Have a willingness to commit to regular monitoring and adjustments under medical supervision to ensure safety and optimal outcomes
Why Therapeutic Peptides Are Gaining Traction In Modern Weight Management
As the science of metabolic medicine evolves, therapeutic peptides are increasingly recognized not just for their potency but for their precision and adaptability. The following key attributes explain why many are turning to peptides for weight management:
1. Safe & Tailored Dosing
Prescribed under professional guidance, these lab-engineered peptides allow tailored dose adjustments and measurable effects. This ensures safety, consistency, and results suited to individual needs, while supporting consistent weight management progress. Additionally, personalized dosing helps minimize adverse reactions and aligns treatment with ongoing health metrics.
2. Synergy With Lifestyle
Peptides work best when combined with proper nutrition, regular exercise, and healthy lifestyle habits. When supported by these interventions, they can enhance energy regulation, improve satiety, and help preserve muscle mass during weight loss.
3. Versatility
Different peptides or combinations can be selected based on your metabolic profile, insulin sensitivity, and body fat distribution, making the approach highly personalized. This flexibility allows clinicians to target specific weight-loss goals (such as reducing visceral fat or supporting lean body mass) tailoring therapy to the unique physiology of each individual.
4. Lower Side Effects
Designed to mimic natural hormones that regulate appetite and energy, peptides often require smaller doses and may cause fewer side effects than traditional medicines. By aligning more closely with the body’s natural signaling pathways, they tend to be better tolerated. This reduces gastrointestinal discomfort or other systemic issues that can interfere with adherence.
It’s worth noting that peptide therapy should always be used under the supervision of a qualified healthcare professional. Individual results may vary, and not all peptides are approved or suitable for every person. Always consult your physician before beginning any new treatment.
The Best Peptides For Weight Loss: A Research-Based Breakdown
Here’s a look at the top peptide-based treatments for weight loss, from those already FDA-approved, to the newer ones still being tested in advanced trials. Each class builds on the science of the one before it, aiming to improve results and reduce side effects.
1. Single-Target Peptides (GLP-1 Receptor Agonists)
The first and most established class is the GLP-1 receptor agonists (glucagon-like peptide-1). Initially developed for diabetes, they help by mimicking a natural gut hormone released after meals — one that signals fullness, slows digestion, and helps control blood sugar levels. Due to this, they make you feel satisfied with less food and promote weight loss steadily.
Their long-term data, proven safety record, and physician familiarity make them an ideal starting point for most individuals. The following are the two FDA-approved best peptides for weight loss:
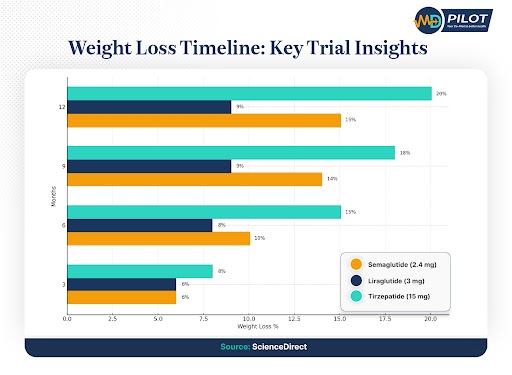
| Type Of Peptide Therapy | Semaglutide | Liraglutide |
|---|---|---|
| FDA-Approved Brand | Wegovy | Saxenda |
| Key Evidence & Outcome | 2.4 mg once weekly resulted in up to 13.9% body weight loss after 68 weeks | 3 mg once daily showed up to 5.8% weight loss over 26 weeks |
| Notable Advantages | Cardiovascular benefit, well-studied safety, approved in many locales | Established track record and daily dosing allowing finer titration |
| Considerations | Gastrointestinal (GI) side effects (such as diarrhea, nausea, constipation, and vomiting), cost, and long-term adherence | More frequent injections, somewhat lower efficacy, GI side effects (such as nausea, diarrhea, and vomiting) |
GLP-1 receptor agonists laid the groundwork for modern peptide therapy—proving that hormonal signaling can safely and effectively drive fat reduction. Their success opened the door for more advanced and multi-pathway innovations that followed.
2. Dual Agonist Peptides (GLP-1 + GIP)
Building on GLP-1 therapy, the next step in peptide development combines two natural hormone signals instead of one. These newer options enhance the same “fullness” effect of GLP-1 peptides while adding another layer of metabolic support, helping the body burn calories more efficiently.
As one of the best peptides for weight loss, they are typically suited for people seeking more significant results or those who haven’t responded fully to single-action peptides. The overview of the only FDA-approved dual agonist peptide is as follows:
| Type Of Peptide Therapy | Tirzepatide |
|---|---|
| FDA-Approved Brand | Zepbound |
| Key Evidence & Outcome | 15 mg once weekly resulted in up to 17.8% body weight loss after 72 weeks |
| Notable Advantages | Potent dual mechanism and more substantial weight loss |
| Considerations | Common GI side effects, gallbladder problems, kidney issues, and allergic reactions |
By activating both GLP-1 and GIP receptors, dual agonists like Tirzepatide deliver deeper metabolic improvements and greater fat reduction. They represent the next logical progression from single-target drugs—offering amplified benefits for suitable candidates.
3. Triple-Action Peptides (Under Trial)
Pushing the science even further, researchers are now developing triple-action peptides that target GLP-1, GIP, and glucagon receptors all at once. They aim to target three key hormone pathways that control hunger, fat metabolism, and energy utilization — combining the benefits of earlier generations into a single therapy.
The most promising of these next-generation candidates is Retatrutide, which has already shown exceptional results in clinical research. It is currently in Phase 3 clinical trials — the last major step before approval, where researchers test its safety and effectiveness in larger and more diverse populations.
Before reaching this advanced stage, the previous trial had already demonstrated impressive weight loss results, as shown below:
| Retatrutide Phase 2 Trial Outcome | ||
|---|---|---|
| Dosage | Weight Loss At 24 Weeks | Weight Loss At 48 Weeks |
| 1 mg | ~7.2% | ~8.7% |
| 4 mg | ~12.9% | ~17.1% |
| 8 mg | ~17.3% | ~22.8% |
| 12 mg | ~17.5% | ~24.2% |
Triple-action peptides such as Retatrutide represent the future of weight-loss medicine—delivering multi-hormonal synergy that could redefine medical obesity treatment. While still in trials, their impressive early results signal the next leap forward in both safety and efficacy.
Combination Therapies & Other Experimental Peptides
Beyond the main approved or trial-based therapies, several experimental combinations are showing exciting results in early studies. These investigational therapies represent the next frontier in peptide-based obesity treatment, aiming to refine outcomes beyond current single or dual agonists.
Researchers are working to optimize the balance between effectiveness and safety, offering hope for more personalized and potent options in the future. However, unapproved versions or peptides sold online should be avoided — the FDA has issued warnings about misleading labels and quality risks. Some of the promising options under study are as follows:
1. CagriSema (Semaglutide + Cagrilintide)
This dual-therapy approach combines two powerful agents under development for obesity and type 2 diabetes. CagriSema enhances satiety and reduces appetite more effectively than semaglutide alone.
The peptide-based therapy recently completed the Phase 3A trial — an initial segment of a large-scale Phase 3 trial designed to confirm safety and effectiveness. It demonstrated an average 13.7% reduction in body weight after 68 weeks, underscoring the potential superiority of this therapy over single-peptide therapy.
2. Pemvidutide
Another emerging candidate, Pemvidutide, is a dual-action therapy. Unlike many peptide therapies, it does not require dose titration, which simplifies the administration process. In Phase 2 studies, which tests efficacy and safety in a moderate group of participants, Pemvidutide showed promising weight-loss outcomes. The trial also suggested that it could become a convenient and scalable option once further validated.
3. AMG 133 (Maridebart Cafraglutide)
Representing a next-generation approach, AMG 133 is designed to promote fat loss while preserving muscle. Phase 2 data showed up to 20% weight loss in non-diabetic individuals and around 17% in those with type 2 diabetes after 52 weeks of treatment. This makes it one of the most compelling multi-pathway therapies under investigation.
Risks, Challenges & Optimization Strategies
No medical treatment is flawless, and even the best peptides for weight loss are no exception. Understanding the potential risks and knowing how to manage them effectively is crucial for achieving long-term, sustainable results. Below, we explore the most common challenges and strategies to mitigate them:
1. Gastrointestinal Side Effects
One of the most frequently reported issues with peptides is gastrointestinal discomfort. Symptoms such as nausea, vomiting, diarrhea, constipation, or abdominal pain affect an estimated 78.9–89.7% of users, particularly during the early stages of treatment or dose escalation.
The good news is that these effects are typically short-lived and tend to subside as your body adjusts to them. Most users can comfortably continue their regimen with minimal disruption to daily life. Moreover, you can minimize discomfort by following a few practical strategies:
- Slow Titration: Increase dosage gradually under medical supervision.
- Modify Eating Habits: Opt for smaller, low-fat meals to ease digestion.
- Symptom Control: Use prescribed anti-nausea medications as needed.
2. Lean Muscle Loss & Body Composition Changes
While fat loss is the primary goal, rapid weight reduction can sometimes result in unintended muscle loss. Preserving muscle is crucial not just for strength and appearance, but also for maintaining a healthy metabolism. To counteract this, focus on supporting lean tissue through a balanced diet, regular exercise, and targeted supplementation.
By pairing any one of the best peptides for weight loss with the following lifestyle supports, you can safeguard muscle integrity:
- Adequate Protein Intake: Aim for 2 g of protein per kilogram of body weight daily.
- Balanced Calorie Deficit: Avoid overly aggressive calorie cuts that accelerate muscle breakdown.
- Resistance Training: Incorporate 2–3 strength training sessions per week, targeting major muscle groups.
- Consider Supplementation: Creatine can be beneficial for maintaining muscle during caloric restriction.
3. Weight Regain After Discontinuation
The most significant long-term challenge with peptide-based therapies is sustaining results once treatment stops. Since peptides influence hunger and fat metabolism while active, discontinuation often leads to increased appetite and gradual weight gain.
Preventing relapse requires foresight and a structured maintenance plan that transitions you smoothly off therapy while reinforcing healthy habits. Some of the long-term optimization tips are as follows:
- Commit To Maintenance: Discuss with your provider whether ongoing or tapered dosing is suitable for your goals.
- Stay Consistent: Continue your nutrition and exercise routines to preserve progress.
- Monitor Regularly: Track weight, metabolic health, and body composition over time.
- Seek Professional Support: Maintain check-ins with healthcare and nutrition experts for accountability and guidance.
Lifestyle Tweaks That Supercharge Peptide Results
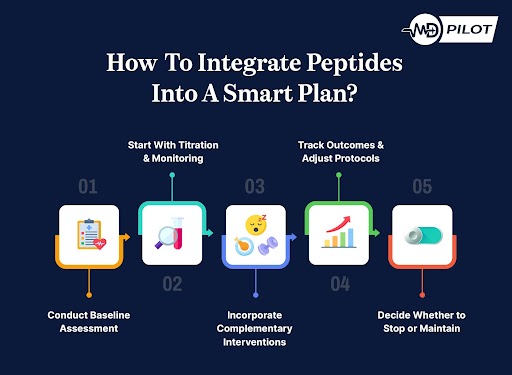
Clinical trials consistently show that combining peptide therapy with structured lifestyle interventions yields significantly better outcomes than medication alone. In fact, a clinical trial on Tirzepatide found that participants who incorporated an intensive lifestyle intervention achieved a body weight reduction of at least 5%. This was in comparison to participants who did not follow the intervention.
This reinforces an important principle: peptides are most effective when integrated into a holistic weight management plan rather than viewed as a standalone solution. Below are the core lifestyle pillars that work synergistically with peptide therapy to maximize body fat loss while maintaining overall metabolic health:
1. Nutritional Strategies
A balanced and intentional approach to nutrition enhances the appetite-suppressing and metabolic effects of peptides. To ensure you can maximize the results of the best peptides for weight loss, keep the following in mind:
- Protein Prioritization: Aim for 20–30% of total calories from protein to preserve lean muscle mass during fat reduction.
- Meal Timing: Establish regular eating patterns that complement the appetite-modulating effects of peptides.
- Mindful Eating: Leverage decreased hunger as an opportunity to develop long-term healthy eating habits.
- Nutrient Density: Focus on foods rich in vitamins, minerals, and antioxidants to prevent nutritional gaps during lower calorie intake.
2. Exercise Programming
Physical activity further enhances the metabolic improvements driven by peptides, promoting fat loss, strength, and cardiovascular health. You can keep yourself in top shape by taking the following steps:
- Resistance Training: Incorporate 3–4 sessions per week to maintain or increase muscle mass.
- Cardiovascular Exercise: Engage in at least 150 minutes of moderate-intensity aerobic activity weekly to boost calorie expenditure and endurance.
- Non-Exercise Activity: Increase daily movement (such as walking, taking the stairs, or doing household chores) to elevate your baseline metabolism.
- Recovery Protocols: Prioritize quality sleep and effective stress management to support hormonal balance and recovery between workouts.
Frequently Asked Questions (FAQs)
Factors such as the type of peptide, dosage, duration, and lifestyle habits all influence outcomes. The following frequently asked questions address common concerns, providing clarity for those considering the best peptides for weight loss to achieve safe and sustainable results.
Clinical trials report a 6–20% reduction in body weight, depending on the peptide used, dosage, duration, and adherence. When considering the best peptides for weight loss, it is essential to remember that individual results vary, and combining therapy with lifestyle adjustments often significantly enhances outcomes.
Most patients require a long-term commitment. Studies indicate substantial weight regain if therapy is discontinued abruptly. Therefore, maintenance or reduced-dose strategies are often recommended. By understanding this, you can plan effective and sustainable interventions, particularly for achieving lasting metabolic and appetite control.
Costs vary widely depending on the country, peptide type, and the level of insurance coverage. Many clinically approved weight-loss peptides are expensive and may only be partially covered by insurance. To manage costs, consider exploring manufacturer assistance, step therapy, or enrollment in clinical trials. Financial planning ensures therapy remains feasible and sustainable.
Stopping therapy abruptly carries a high risk of regaining weight. Most protocols recommend tapering or transitioning to maintenance dosing. This gradual approach helps preserve results, supports metabolic stability, and aligns with evidence-based strategies, ensuring that weight-loss achievements from peptide therapy are more likely to be maintained over time.
Making Smart Weight-Loss Decisions With MD Pilot
Navigating peptides for weight loss can be overwhelming, given the variety of options and potential side effects. Understanding how each peptide works, how dosing should be individualized, and what lifestyle factors influence positive results is essential for achieving effective outcomes.
With the proper knowledge and guidance, you can make informed choices that align with your unique physiology and weight loss goals. That’s where MD Pilot can help. By providing expert-verified medical insights and practical tools, we guide you in evaluating whether peptides—or other interventions—fit your unique health goals.
Our tools, including the Personal Meal Planning Calculator and Personal Portion Calculator, make it easier to identify patterns, take preventive steps, and support healthier choices. With these tools and our blogs, you can manage your weight confidently while protecting your overall well-being.
References:
- Ghusn, W., & Hurtado, M. D. (2024). Glucagon-like Receptor-1 agonists for obesity: Weight loss outcomes, tolerability, side effects, and risks. Obesity Pillars, 12, 100127.
https://www.sciencedirect.com/science/article/pii/S2667368124000299 - Jastreboff, A. M., Kaplan, L. M., Frías, J. P., et al. (2023). Triple-Hormone-Receptor Agonist Retatrutide for Obesity – A Phase 2 Trial. New England Journal of Medicine, 389(6), 514–526.
https://pubmed.ncbi.nlm.nih.gov/37366315/ - Lau, J. L., & Dunn, M. K. (2018). Therapeutic peptides: Historical perspectives, current development trends, and future directions. Bioorganic & Medicinal Chemistry, 26(10), 2700–2707.
https://www.sciencedirect.com/science/article/pii/S0968089617310222 - Moiz, A., Filion, K. B., Toutounchi, H., et al. (2025). Efficacy and Safety of Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss Among Adults Without Diabetes : A Systematic Review of Randomized Controlled Trials. Annals of Internal Medicine, 178(2), 199–217.
https://pubmed.ncbi.nlm.nih.gov/39761578/ - WebMD. (n.d.). Peptides: Types, Uses, and Benefits.
https://www.webmd.com/a-to-z-guides/what-are-peptides - Zheng, B., Wang, X., Guo, M., et al. (2025). Therapeutic Peptides: Recent Advances in Discovery, Synthesis, and Clinical Translation. International Journal of Molecular Sciences, 26(11), 5131.
https://www.mdpi.com/1422-0067/26/11/5131
Disclaimer:
The information provided on MD-Pilot is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recomended Articles
View AllWeekly Health Intel
Get evidence-based health tips, latest research, and exclusive guides delivered weekly




