Understanding Hypoglycemia Shock: Causes, Symptoms, and Treatments
Introduction
Hypoglycemia shock—a condition that sounds as serious as it is—requires our immediate attention. This medical emergency arises when blood sugar levels plummet, leaving the body scrambling to function properly. From dizzying disorientation to downright danger, one might wonder, “How do I prevent a nutritional nosedive?” Here, we’ll explore what triggers hypoglycemia shock, identify those pesky warning signs, and serve up some treatment strategies to manage and prevent life-changing episodes.
Key Takeaways
- Hypoglycemia shock is a severe drop in blood sugar levels requiring urgent medical care.
- Common causes include over-medication, intense exercise, or insufficient dietary intake.
- Symptoms such as confusion, sweating, and palpitations should prompt immediate action.
- Quick treatments include glucose tablets, well-timed snacks, or medical intervention.
Table of Contents
Causes of Hypoglycemia Shock
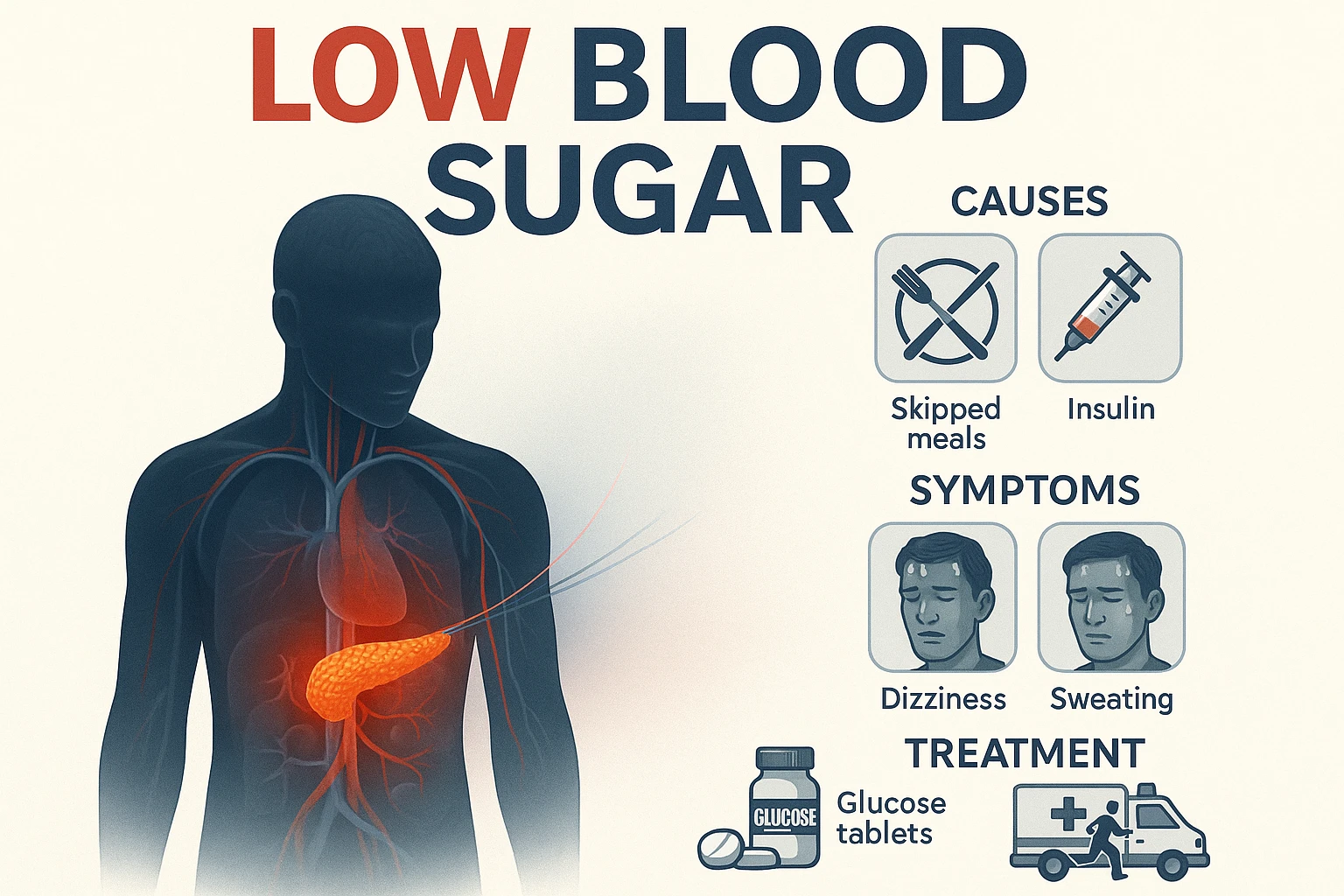
Fasten your seatbelts, we’re diving into the data on hypoglycemia shock causes. This condition emerges when insulin—which is like a conductor orchestrating sugar breakdown—overacts. Common players? Overdose of diabetes medication, skipping meals, or unexpectedly rigorous physical activities. Stunningly, studies show 46% of type 1 diabetes patients experience severe hypoglycemia annually. A sobering statistic!
- Excess insulin dosages can prompt dangerous drops in blood sugar.
- Inadequate carbohydrate intake following workouts makes blood cells cry out for fuel.
- Forgetfulness or delays in scheduled meals can upset bodily regulation.
Recognizing the Symptoms
Picture this: a blood sugar drop leaves one feeling as if suddenly thrust onto a malfunctioning merry-go-round. Recognizing hypoglycemia shock symptoms is crucial! Initial signs include lightheadedness, excessive sweating, and—brace yourselves—heart-pounding palpitations. According to research conducted among hospitalized patients, timely identification can save lives.
- Feelings of shakiness and anxiety are immediate red flags.
- Irrational confusion or vision disturbances shouldn’t be ignored.
- Severe cases may see individuals losing consciousness—a wake-up call for urgent intervention.
Effective Treatment Options
But wait, the science serves up a surprising side dish. Immediate glucose intake can ameliorate urgent symptoms of hypoglycemia shock. Reach for quick-dissolving glucose tablets or sugary drinks to stabilize blood sugar. In more stubborn cases, professional medical assistance—like an intravenous glucose drip—may be necessary.
- Administer glucose tablets for 15-minute symptom assessment.
- Incorporate rapid-digesting carbs post-exercise to maintain balance.
- Do not skip follow-ups if warning signs persist!
Prevention Strategies
Here’s what the research actually shows: consistent monitoring and preventive habits can keep hypoglycemia shock at bay. From community-wide strategies like deploying glucagon kits in public spaces to embracing technology, there is safety in awareness. Adopting such practices can prevent emergencies before they strike.
- Utilize continuous glucose monitors for real-time sugar level insights.
- Carry fast-acting carbs at all times, lest an “uh-oh” moment arises.
- Coordinate with healthcare providers for personalized management plans.
FAQs
- Q: Can hypoglycemia shock occur without diabetes?
A: Yes, non-diabetics can experience hypoglycemia due to factors like prolonged fasting or alcohol consumption. - Q: What should I do if someone shows signs of hypoglycemia shock?
A: Offer them a carbohydrate-rich snack and monitor; if severe, seek emergency medical help immediately. - Q: Are there long-term effects of repeated hypoglycemic events?
A: Recurrent episodes can escalate to further complications, including cognitive impairment over time.
Conclusion
And now, for a dash of nutritional clarity: understanding and managing hypoglycemia shock requires a well-balanced mix of awareness and preparedness. From monitoring blood sugar levels diligently to ensuring those around you know the signs of low sugar drops, your “plate” should be full of these prolific insights. So, fend off the “monster of the midnight snack” and keep those sugar levels just right—with every meal or emergency snack, you’re crafting a safer, sweeter future for yourselves and loved ones!

Leave a Reply